Giovanna Mallucci facts for kids
Quick facts for kids
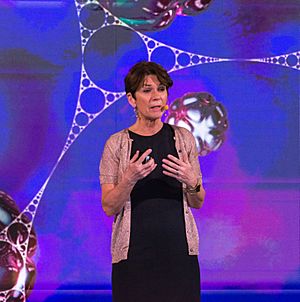
Giovanna Mallucci
|
|
|---|---|
 |
|
| Born | 29 June 1963 |
| Alma mater | St Hilda's College, Oxford University College London Imperial College London |
| Known for | mechanisms of neurogenerative diseases; translational neuroscience |
| Awards | Potamkin Prize (2021) |
| Scientific career | |
| Fields | Neuroscience Neurodegeneration Prion diseases |
| Institutions | University of Cambridge University of Leicester |
| Thesis | Prion protein gene knockout in the mouse using the Cre/1oxP system (2001) |
Giovanna Rachele Mallucci (born 29 June 1963) is a British doctor and brain scientist. She studies how our brains work and what happens when they get sick.
Currently, she is a lead scientist at Altos Labs in Cambridge, UK. Before that, she was a director at the UK Dementia Research Institute. She also taught about brain science at the University of Cambridge. Dr. Mallucci is an expert in diseases that affect the brain over time, like neurodegenerative diseases.
Contents
Learning About the Brain
Giovanna Mallucci went to Haberdashers' Aske's School for Girls. She studied how the body works at the University of Oxford. Later, she became a doctor at University College London.
In 2001, she earned her PhD from the University of London. This means she did a lot of research and became an expert in her field. She then specialized in neurology, which is the study of the nervous system.
Her Work and Discoveries
Dr. Mallucci has held many important jobs during her career. From 2017 to 2022, she led the UK Dementia Research Institute at the University of Cambridge. She also taught as a professor there.
She was also a special doctor at Addenbrooke's Hospital, Cambridge. Before that, she worked at the MRC Toxicology Unit in Leicester. There, she led the neurobiology department and was a professor of neuroscience.
Dr. Mallucci also helps edit important science journals like Brain. This means she helps decide which new research gets published.
Understanding Brain Diseases
Dr. Mallucci has made amazing discoveries about brain diseases. She studies how proteins in the brain can fold incorrectly. This can cause problems like neurodegeneration.
She found that early brain damage might sometimes be fixed. She also learned how a process called the unfolded protein response (UPR) can harm brain cells. This UPR is a way cells react to stress.
New Ways to Help Brains
Her work showed that changing the UPR could help prevent brain damage. She found the first medicine that could stop neurodegeneration. She also found existing medicines that could be used for this purpose. These medicines are now being tested in people.
She also discovered that a special protein called RBM3 helps brain connections grow back. These connections are called synapses. Her research gives new hope for treating diseases like dementia.
Awards and Honors
Dr. Mallucci has received many awards for her important work.
- Potamkin Prize (2021)
- Masland Award Medal, World Congress of Neurology (2021)
- Fellow of the Academy of Medical Sciences (2017)
- Frank May Medal for Excellence in Research (2012)
- President’s Prize in Clinical Neuroscience (2004)
- Queen Square Prize in Neurology (2003)

