Insulin pump facts for kids
Quick facts for kids Insulin pump |
|
|---|---|
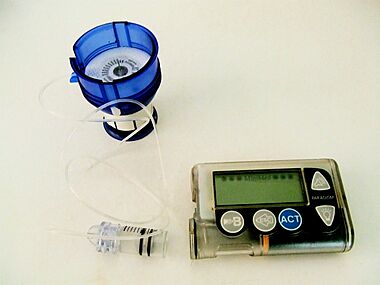
Paradigm insulin pump 530g, showing an infusion set loaded into spring-loaded insertion device called serter. A reservoir is attached to the infusion set (shown here removed from the pump).
|
|
| Specialty | {{#statements:P1995}} |
An insulin pump is a small medical device. It helps people with diabetes get the insulin they need. It gives insulin continuously, right under the skin. This is also called continuous subcutaneous insulin therapy.
Insulin pumps come in different designs. A common pump has a main part with controls and batteries. Inside, there's a small container for insulin. A thin tube connects this container to a tiny needle, called a cannula. This cannula goes just under your skin. Some newer pumps are smaller. They might not have tubes, like "patch pumps." These stick right onto your skin.
Using an insulin pump is another way to get insulin. It's an alternative to daily shots with insulin pens or syringes. Pumps allow for more flexible insulin use. This works best when you also check your blood glucose and count carbohydrates in your food.
Contents
How Insulin Pumps Help
Insulin pumps give insulin all the time. They are mainly used by people with type I diabetes.
Benefits of Using a Pump
- Many users say their quality of life is better. This is true for people with type 1 and some with type 2 diabetes.
- Pumps use fast-acting insulin for your daily needs. This means you can be more flexible with meals and exercise. You don't need a strict schedule like with slow-acting insulin.
- You can program the pump to give different amounts of insulin. This helps control blood sugar at different times of the day. It can prevent low blood sugar during the night, especially from the dawn phenomenon.
- Many people find giving insulin with a pump easier. It can also be more private than giving a shot.
- Pumps can give very exact amounts of insulin. This helps keep blood sugar and HbA1c levels more stable. It can lower the risk of long-term problems from diabetes.
- Many modern pumps have a "bolus wizard." This smart tool figures out how much insulin you need. It considers your food, blood sugar, and insulin already working in your body.
- Insulin pumps keep a record of how much insulin you use. You can upload this history to a computer. This helps you see trends and understand your insulin needs.
- Some studies show pumps can help with nerve pain. This pain is a common problem from diabetes.
Challenges of Using a Pump
- Insulin pumps and their supplies can be expensive. They cost more than syringes for shots.
- There's a higher risk of diabetic ketoacidosis if the pump stops working. This can happen if the battery dies or the insulin gets too hot. It can also happen if the tube leaks or the needle bends. Pump users often check their blood sugar more often to make sure the pump is working.
- You need to wear the pump most of the time. This means you need ways to protect it during sports or swimming. Some people might find wearing the pump and its tubes uncomfortable.
- Sometimes, scar tissue can build up where the needle goes under the skin. This can make it harder to find good spots to wear the pump over time. Areas with scar tissue might also need more insulin.
- Some users might have skin irritation from the adhesive on the infusion set. This can depend on the person and the pump brand.
- You might need more insulin supplies overall. Some insulin can be wasted when refilling the pump or changing the infusion site.
- In 2005, a safety warning was issued about pumps that rely on smartphones. Some people missed important alerts due to phone settings.
Getting a Pump
More people are using insulin pumps because:
- They make it easy to give many small insulin doses. This is helpful for intensive insulin therapy.
- They can give very tiny doses, which is good for babies.
- Doctors and insurance companies support them more. This is because pumps help reduce long-term diabetes problems.
- Blood glucose monitoring has improved. Newer meters need smaller blood drops and are less painful.
History of Insulin Pumps
In the early 1960s, Dr. Arnold Kadish made a device to control blood sugar. It was very big, like a backpack. It was never sold to the public.
In 1976, the first commercial insulin pump was created. It was called the Biostator. This pump was very large, weighing 60 kg (about 130 pounds). It could also check blood sugar levels.
Between 1978 and 1988, Robert Channon developed smaller insulin pumps. Today, insulin pumps are tiny. They can fit in a pocket or purse.
In 1984, an Infusaid pump was put inside a patient's body. This was a successful treatment.
The use of insulin pumps was first supported in the United Kingdom in 2003. This was by the National Institute for Health and Care Excellence (NICE).
Smart Pump Features
New insulin pumps are becoming "smart." They have features that make giving insulin easier.
- Insulin on board: The pump estimates how much insulin is still working in your body. This helps you avoid giving too much insulin if you need another dose.
- Bolus calculators: The pump helps you figure out the right insulin dose. You enter the carbs you'll eat, and the "wizard" suggests the insulin needed. It also considers your current blood sugar.
- Custom alarms: The pump can remind you about important actions. For example, it can alarm if you miss a meal dose or a blood sugar test.
- Touch bolus: This feature helps people with vision problems. You can give insulin without looking at the screen. Beeps confirm the dose.
- Computer connection: Most pumps can connect to computers. This helps you keep records and manage your pump settings.
- Blood glucose meter link: You can manually enter blood sugar data into the pump. Some pumps can even connect directly to a blood glucose meter.
- Continuous glucose monitoring (CGM) link: Some pumps can show your glucose levels from a CGM system.
Future Pump Ideas
- Combining pumps with continuous glucose monitoring systems. This could lead to an artificial pancreas. This system would automatically control insulin based on blood sugar levels.
- Pumps that give other medicines, like pramlintide. This could help control blood sugar better after meals.
- Pumps that can give both insulin and glucagon. Glucagon helps raise blood sugar if it gets too low. This would be very useful in an artificial pancreas system.
- Faster-acting insulins. These insulins would work more quickly. This could help them match meals better and fix high blood sugar faster.
How Insulin is Given
An insulin pump uses only fast-acting insulin. It gives insulin in two main ways:
- A bolus dose: This is a larger dose given to cover food or to lower high blood sugar.
- A basal dose: This is a small, continuous amount of insulin. It's given all day and night to cover your body's basic needs between meals.
Bolus Shapes
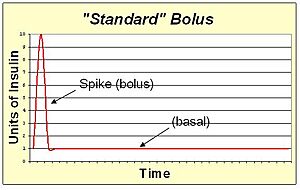
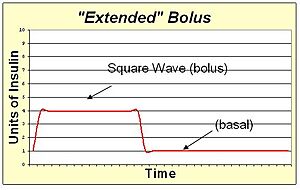
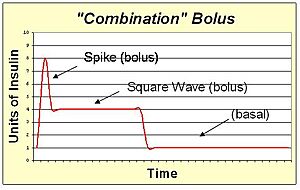
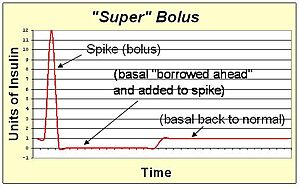
Pump users can change how a bolus is delivered. This is called "shaping the bolus." It helps control blood sugar better for different foods.
- A standard bolus gives all the insulin at once. It's like a quick shot. This works best for meals high in carbs but low in fat and protein.
- An extended bolus gives insulin slowly over time. This avoids a big rush of insulin. It's good for meals high in fat and protein, like steak, which raise blood sugar for many hours. It also helps if your digestion is slow.
- A combination bolus mixes a quick dose with a slow, extended dose. This is good for meals that are high in both carbs and fat, like pizza or chocolate cake.
- A super bolus makes the quick dose even stronger. It "borrows" some of your continuous basal insulin. This helps attack a big blood sugar spike very quickly, like after sugary cereals.
Bolus Timing
You manually start a bolus with a pump. This lets you "pre-bolus" to help prevent high blood sugar after eating. A pre-bolus means giving insulin before you eat.
Pre-bolusing is helpful in two cases:
- For high-sugar foods: Fast-acting insulin takes about 15-20 minutes to start working. Sugary foods hit your bloodstream faster. Pre-bolusing helps the insulin start working when the sugar arrives.
- When blood sugar is high before a meal: You can give insulin earlier. This helps bring down your blood sugar before eating raises it again.
Sometimes, it's better to give insulin after you start eating. This might be if your blood sugar is low or if you're eating low-sugar foods. Your blood sugar, food type, and how your body reacts all affect the best time to bolus.
Basal Rate Patterns
You can also customize your continuous basal insulin. This helps match your body's needs throughout the day.
- Lower basal rates at night can prevent low blood sugar in young children.
- Higher basal rates at night can help teenagers. This is because growth hormones can raise blood sugar.
- An increase before dawn can prevent high blood sugar from the dawn effect in adults and teens.
- You can plan for regular exercise, like gym class or sports.
How to Figure Out Basal Rates
Your basal insulin needs change. They vary from person to person and throughout the day. To find your basal rate, you fast (don't eat) and check your blood sugar often. You shouldn't eat or take bolus insulin for at least 4 hours before or during this time. If your blood sugar changes a lot, you adjust the basal rate. The goal is to keep your blood sugar steady.
For example, to find your morning basal rate, you would skip breakfast. You'd check your blood sugar from waking until lunch. You repeat this over several days. Once your basal rate matches your needs, you can be flexible. You can sleep in or work late without worrying about meals.
Many things can change your insulin needs:
- The "honeymoon period" after a type 1 diabetes diagnosis.
- Growth spurts, especially during puberty.
- Weight changes.
- Medicines that affect insulin (like corticosteroids).
- Changes in your routine (eating, sleeping, exercise).
- When your blood sugar control gets worse.
- Changes in seasons.
Your diabetes doctor or nurse should teach you about basal rates. This should happen before you start pump therapy.
Temporary Basal Rates
Since the pump uses fast-acting insulin, you can quickly change your basal rate. This is called a temporary basal rate. It's helpful for:
- Long car rides, when you're not active.
- During or after sports, when your body needs less insulin.
- When you are sick or stressed. Your insulin needs might go up.
- When you have ketones in your blood. You might need more insulin.
- During long fasts, like for religious reasons. Your insulin needs might be lower.
- During menses, when you might need more insulin.
Security Concerns
In 2011, a researcher showed a security problem with insulin pumps. He could hack the wireless system used to control the pump. A pump maker, Medtronic, later confirmed a flaw in its pumps that could be used by others.
See also
 In Spanish: Bomba de insulina para niños
In Spanish: Bomba de insulina para niños
- Automated insulin delivery system
- Continuous glucose monitor
- Minimed Paradigm
 | Emma Amos |
 | Edward Mitchell Bannister |
 | Larry D. Alexander |
 | Ernie Barnes |