Ralph M. Steinman facts for kids
Quick facts for kids
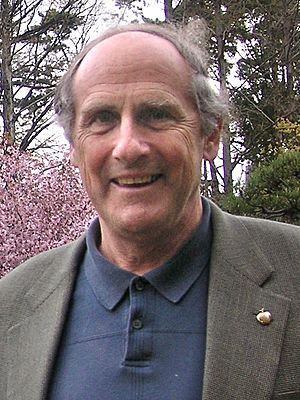
Ralph M. Steinman
|
|
|---|---|
 |
|
| Born |
Ralph Marvin Steinman
January 14, 1943 Montreal, Quebec, Canada
|
| Died | September 30, 2011 (aged 68) Manhattan, New York, U.S.
|
| Alma mater | McGill University (B.S., 1963) Harvard University (M.D., 1968) |
| Known for | Discovery of dendritic cells and its role in adaptive immunity |
| Spouse(s) | Claudia Hoeffel (3 children) |
| Awards | Robert Koch Prize (1999) Gairdner Foundation International Award (2003) Nobel Prize in Physiology or Medicine (2011) |
| Scientific career | |
| Fields | Immunology Cell Biology |
| Institutions | Rockefeller University in New York City |
| Academic advisors | Elizabeth Hay (Harvard) James G. Hirsch and Zanvil A. Cohn (Rockefeller University) |
| Influenced | Romina Goldszmid |
Ralph Marvin Steinman (born January 14, 1943 – died September 30, 2011) was a Canadian doctor and medical scientist. He worked at Rockefeller University in New York. In 1973, he discovered and named dendritic cells. These are special cells that help our bodies fight off sickness. Steinman won the 2011 Nobel Prize in Physiology or Medicine for this important discovery.
Contents
Early Life and Education
Ralph Steinman was born in Montreal, Canada. His family was Jewish, and he was one of four children. When he was young, his family moved to Sherbrooke, where his father ran a clothing store.
After high school, Ralph went back to Montreal. He earned a science degree from McGill University. Later, he studied medicine at Harvard Medical School, finishing in 1968. He then did his internship and residency at Massachusetts General Hospital.
Winning the Nobel Prize
On October 3, 2011, Ralph Steinman was announced as a winner of the Nobel Prize in Physiology or Medicine. He received half of the prize for finding dendritic cells and showing how they help our body's defense system. The other half went to two other scientists, Bruce Beutler and Jules A. Hoffmann, for their work on how our body first reacts to germs.
However, there was a problem. The Nobel Committee did not know that Ralph Steinman had passed away three days earlier, on September 30. He died from pancreatic cancer. Usually, the Nobel Prize is not given to someone after they have died. But because the decision was made before they knew he had passed, the committee decided to let the award stand.
Ralph's daughter shared that he had joked about staying alive until the prize was announced. He said, "I know I have got to hold out for that. They don't give it to you if you have passed away. I got to hold out for that."
Ralph Steinman received many other awards for his work on dendritic cells during his life. These included the Albert Lasker Award For Basic Medical Research in 2007 and the Gairdner Foundation International Award in 2003. In 2016, a new street in Sherbrooke, Quebec, was named "rue Ralph Steinman" to honor him.
Other Awards and Honors
- 1998 – William B. Coley Award
- 1999 – Robert Koch Prize
- 2003 – Gairdner Foundation International Award
- 2006 – Debrecen Award for Molecular Medicine
- 2007 – Albert Lasker Award for Basic Medical Research
- 2009 – Albany Medical Center Prize
- 2010 – Heineken Prizes
- 2011 – Nobel Prize in Physiology or Medicine
Understanding Immunity: Ralph Steinman's Research
Ralph Steinman's research was about immunology. This is the study of how our bodies fight off infections and diseases. Our body has two main ways to protect itself:
- Innate immunity: This is our body's first, quick defense against germs. It doesn't remember past infections.
- Adaptive immunity: This defense system learns and remembers germs. If you get sick with the same germ again, your adaptive immunity can fight it off faster.
Scientists had two main ideas about how immunity worked. They thought that certain cells called macrophages helped with the first defense. They also believed that special proteins called antibodies helped with the adaptive defense.
Ralph Steinman discovered that dendritic cells are the missing link between these two types of immunity. He found that these cells connect the body's first defense to its smarter, memory-based defense.
How Dendritic Cells Work
Steinman studied how our body starts to make antibodies in a lab. He found that antigens (parts of germs), lymphocytes (a type of white blood cell), and "accessory cells" all work together to create an immune response. Among these accessory cells, he found a new type of cell with "dendrites," which are like tiny arms. These were the dendritic cells.
He learned that dendritic cells have special features. Unlike macrophages, they don't constantly "eat" germs. Instead, they are very good at capturing, processing, and showing parts of germs to other immune cells. This "showing" process is key to starting the adaptive immune response.
Dendritic cells help our body's T cells, which are important fighters in our immune system. They act like "nature's helpers" for T cell immunity. They can also make helpful substances like cytokines, which are signals that tell other immune cells what to do.
When dendritic cells find germs, they change and become "mature." This change helps them tell the T cells exactly what kind of germ they've found. This way, the T cells can create the right kind of defense. Dendritic cells are found all over the body, especially in places where immune responses begin.
See also
 In Spanish: Ralph M. Steinman para niños
In Spanish: Ralph M. Steinman para niños
- List of Jewish Nobel laureates
 | Anna J. Cooper |
 | Mary McLeod Bethune |
 | Lillie Mae Bradford |

