Tissue typing facts for kids
Tissue typing is a way to check if the body parts (tissues) of a person who wants to donate an organ are a good match for the person who needs it. This check is done before an organ transplant. If the tissues don't match well, the body of the person getting the organ might reject it. There are different ways to do tissue typing.
What is Tissue Typing?
During tissue typing, scientists look for special markers on a person's cells called human leukocyte antigens (HLAs). Think of HLAs as unique ID badges on the surface of our cells. They help our immune system tell the difference between our own cells and foreign cells.
If the HLA markers from a donor organ don't match the recipient's own HLA markers, the recipient's immune system might see the new organ as an enemy. This can cause the body to fight against the new organ.
When HLA markers don't match, the recipient's body can make special "attack" proteins called donor-specific antibodies (DSAs). These DSAs can lead to the body rejecting the new organ. If the donor and recipient HLAs are a good match, the new organ is much more likely to be accepted by the recipient's body.
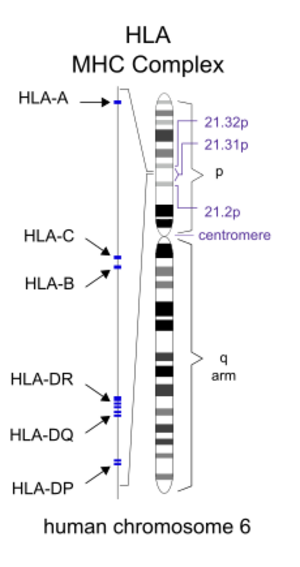
Scientists check many different HLA genes in both the donor and recipient. These include HLA Class I genes like A, B, and C, and HLA Class II genes like DRB1, DRB3, DRB4, DRB5, DQA1, DQB1, DPA1, and DPB1. It's tricky to match HLAs because the HLA area in our DNA is the most varied part of the human body.
How is Tissue Typing Done?
One of the first ways to do tissue typing was called serological typing. In this method, a donor's blood cells are mixed with special liquids (serum) that contain antibodies against different HLA types.
If the antibodies recognize the HLA markers on the donor's cells, a process called complement activation happens. This causes the cells to break open (lysis) and die. When the cells break open, they can take in a special blue dye. This helps scientists figure out the HLA type of the cells based on which antibodies caused the cells to break.
This method was used a lot because it was simple, fast, and cheap. However, there are so many different HLA types that it was often hard to find the exact antibodies needed. Serological typing also didn't give a very clear picture of all the HLA markers. Because of this, many labs now use newer, better methods.
More recently, better ways to do tissue typing have been developed. These include methods that use PCR, which is a way to make many copies of DNA. Some PCR methods use special starting pieces called sequence-specific primers (SSP) or tiny DNA probes called sequence-specific oligonucleotide probes (SSOP).
SSP-PCR can take a lot of time and resources. SSOP-PCR is better for checking many people at once, like for bone marrow donor lists. Another PCR method, RT-PCR, is fast and flexible, but it can be expensive.
Another method for HLA typing is called Reference Strand-Mediated Conformational Analysis (RSCA). In this method, an unknown HLA sample is mixed with a known HLA sample. Then, they are separated using a technique called electrophoresis. RSCA has limits because there aren't enough known HLA samples to compare against all the different types.
Currently, the best way to do HLA typing is by directly reading the DNA code, which is called DNA sequencing. This can be done using methods like Sanger sequencing or next generation sequencing. While these methods are very good, they can also take a lot of time and are more expensive. RNA sequencing can also be used, but many labs don't use it because RNA is not as stable as DNA and can break down easily.
See also
- Graft-versus-host disease
- Histocompatibility
 | May Edward Chinn |
 | Rebecca Cole |
 | Alexa Canady |
 | Dorothy Lavinia Brown |