Frostbite facts for kids
Quick facts for kids Frostbite |
|
|---|---|
| Synonyms | Frostnip |
 |
|
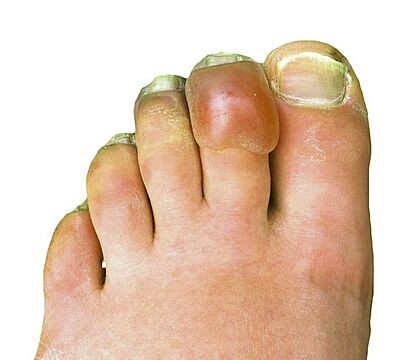
| Frostbitten toes two to three days after mountain climbing | |
| Symptoms | Numbness, feeling cold, clumsiness, pale color |
| Complications | Hypothermia, compartment syndrome |
| Types | Superficial, deep |
| Causes | Temperatures below freezing |
| Risk factors | Alcohol, smoking, mental health problems, certain medications, prior cold injury |
| Diagnostic method | Based on symptoms |
| Similar conditions | Frostnip, pernio, trench foot |
| Prevention | Avoid cold, wear proper clothing, maintain hydration and nutrition, stay active without becoming exhausted |
| Treatment | Rewarming, medication, surgery |
| Medication | Ibuprofen, tetanus vaccine, iloprost, thrombolytics |
| Frequency | Unknown |
Frostbite is a serious skin injury that happens when your body parts get too cold and freeze. It's like ice forming inside your skin or other tissues. This usually affects your fingers, toes, nose, ears, cheeks, and chin. Most often, it happens to your hands and feet.
When you first get frostbite, your skin might feel cold, tingly, or numb. It might also look white or bluish, and you could feel clumsy. After treatment, the area might swell or get blisters. Sometimes, serious problems like hypothermia (when your whole body gets too cold) can happen.
People who spend a long time in very cold places are most at risk. This includes winter sports fans or people who don't have warm homes. Other things that increase risk include certain health issues or past cold injuries. Frostbite happens because ice crystals form in your tissues. These crystals can damage small blood vessels. Doctors usually diagnose frostbite based on your symptoms. It can be mild (superficial) or severe (deep).
You can prevent frostbite by wearing warm, covering clothes. Try to avoid very cold temperatures and strong winds. Make sure you drink enough water and eat well. Staying active can help keep you warm, but don't get too tired. If someone has frostbite, they need to be warmed up carefully. This can be done by putting the affected part in warm water. It's important not to rub the area, as this can cause more damage. Sometimes, medicine or even surgery is needed for severe cases.
People have known about frostbite for thousands of years. Evidence of it was found on a mummy from the Andes mountains, dating back 5,000 years! It has also affected many soldiers in wars throughout history.
Contents
What is Frostbite?
Frostbite happens when parts of your body, like your cheeks, ears, nose, fingers, and toes, get so cold that they freeze. Before frostbite, you might get "frostnip," which is a milder cold injury. The longer you stay in the cold, the worse frostbite can get. Doctors classify frostbite by how deep the injury is, similar to how burns are classified.
Mild Frostbite: First Degree
- First degree frostbite is a mild injury to the surface of your skin. It usually doesn't cause lasting damage.
- The main sign is that you lose feeling in the skin. The area feels numb and might be a bit swollen. It might also have a red border.
- A few weeks later, the top layer of skin might peel off.
Moderate Frostbite: Second Degree
- In second degree frostbite, clear blisters appear on the skin early on. The skin surface also becomes hard.
- Later, this hard, blistered skin dries out, turns black, and peels away.
- At this stage, you might have lasting sensitivity to cold and numbness.
Severe Frostbite: Third Degree
- Third degree frostbite means the tissues below your skin have frozen.
- You might see blood blisters and the skin can turn a "blue-grey" color.
- The pain can last for weeks, and a black crust forms on the skin.
- This type of frostbite can cause long-term damage and even affect growth plates in children.
Very Severe Frostbite: Fourth Degree
- Fourth degree frostbite affects deeper parts of the body, like muscles, tendons, and even bone.
- Early on, the skin looks colorless and feels very hard. Strangely, it might not hurt when it warms up.
- Later, the skin turns black and becomes dry, like a mummy. It can take a month or more to know how much permanent damage there is. Sometimes, the damaged part can fall off on its own after a couple of months.
Why Does Frostbite Happen?
Frostbite is mainly caused by being exposed to very cold temperatures.
Things That Increase Risk
- Cold Exposure: Being in cold places for too long, whether for work, fun, or because of where you live, is the biggest risk.
- Not Enough Warmth: Wearing clothes that aren't warm enough or not having proper shelter makes frostbite more likely.
- Body's Heat: Frostbite is more common when your body can't make or keep enough heat.
- Physical Factors: Not moving much or being stressed (like not eating or drinking enough) can also increase your risk.
- Health Conditions: Some health problems, like diabetes or Raynaud's phenomenon, can affect your blood flow and make you more prone to frostbite.
- Substances: Certain substances can also affect your circulation.
How Frostbite Affects Your Body
Understanding how frostbite works helps us prevent and treat it.
When Your Body Freezes
- When you get cold, your blood vessels get narrower. This is called vasoconstriction.
- If temperatures drop below about -2°C (28°F), ice crystals can start to form in your tissues. Below -4°C (25°F), ice can even form in your blood.
- These ice crystals can damage the tiny blood vessels where the injury happens. Frostbite usually occurs when temperatures are below about -0.55°C (31°F).
When Your Body Warms Up
- Surprisingly, warming up after frostbite can also cause damage. This is called "reperfusion injury."
- It involves blood vessels widening, swelling, and poor blood flow.
- Small blood clots can also form. Blisters and blood vessel spasms can happen after the area warms up.
Stages of Injury
Frostbite damages body tissue in four main stages:
- Prefreeze: Tissues get cold, but no ice crystals have formed yet.
- Freeze-Thaw: Ice crystals form, which damages and kills cells.
- Vascular Stasis: Blood starts to clot or leak out of the blood vessels.
- Late Ischemic: This stage involves inflammation, lack of blood flow, and tissue death.
How Doctors Diagnose Frostbite
Doctors diagnose frostbite by looking at your signs and symptoms and asking about your recent activities.
- Frostnip: This is similar to frostbite but less severe. No ice crystals form in the skin. The skin turns white and numb, but it quickly gets better after warming up.
- Trench Foot: This is damage to nerves and blood vessels from being in cold, wet (but not freezing) conditions for a long time. It can get better if treated early.
- Pernio (Chilblains): This is skin inflammation from being exposed to wet, cold (but not freezing) conditions. It can cause different types of sores and blisters.
- Other Conditions: Some other conditions can look like frostbite, but they are not caused by cold.
- Hypothermia: People with hypothermia (when the whole body is dangerously cold) often have frostbite too. Since hypothermia is life-threatening, doctors treat it first.
How to Prevent Frostbite
Preventing frostbite is very important!
- Cover Up: Always cover your skin and head, especially in cold weather.
- Eat and Drink: Make sure you eat enough and stay hydrated.
- Proper Footwear: Wear shoes and boots that aren't too tight, as this can cut off circulation.
- Stay Active: Keep moving to stay warm, but don't get so tired that you can't keep warm.
- Avoid Moisture: Keep your skin dry. Sweat or wet clothes can make you colder.
- Layer Clothes: Wear several layers of clothing. This traps warm air and keeps you warmer.
- Warming Devices: Use hand warmers or electric warming devices if you have them.
- Recognize Early Signs: Learn the early signs of frostnip and frostbite so you can get warm quickly.
- Avoid Extreme Cold: Try to avoid temperatures below about -23°C (-9°F).
Treating Frostbite
If you or someone you know might have frostbite, it's important to get to a warm, safe place right away.
- Get Warm: Drink warm fluids. If there's no chance of the area refreezing, you can warm the affected body part by putting it under a companion's arm.
- Don't Refreeze: If the area might refreeze, do NOT warm it up. Get to a medical facility as quickly as possible without warming the area. Refreezing can cause much worse damage.
- No Rubbing: Do not rub the affected area. This can cause more tissue damage.
- Pain Relief: Medicines like ibuprofen can help with pain and swelling.
- First Priority: For people with frostbite, the first thing doctors check for is hypothermia, which is more dangerous. Your body's core temperature should be above 35°C (95°F) before treating frostbite.
- Fluids: You might be given fluids to drink or through an IV.
Rewarming in the Hospital
- If the area is still frozen, doctors will warm it up quickly in a warm bath. The water should be around 37–39°C (98.6–102.2°F).
- Fast thawing helps reduce tissue damage.
- Rewarming can be very painful, so pain medicine is important.
Medications for Severe Cases
- For very severe frostbite, especially if there's a risk of losing a limb, doctors might use special medications.
- These medicines, like iloprost, can help open up blood vessels and prevent blockages. This treatment is often used within 48 hours of the injury.
Surgery for Frostbite
- Sometimes, surgery is needed for frostbite, depending on how bad the damage is.
- Doctors usually wait to remove dead tissue unless there's a serious infection. This is why people say, "Frozen in January, amputate in July," meaning they wait to see what tissue will survive.
- If swelling causes too much pressure, a surgery called fasciotomy might be done to save blood flow.
What Happens After Frostbite?
After frostbite, some tissue might be lost, or parts of the body might fall off on their own.
- Nerve Damage: Permanent nerve damage, like loss of feeling, can happen.
- Healing Time: It can take several weeks to know which parts of the tissue will survive.
- Exposure Time: How long you were exposed to the cold is more important than how cold it was.
- Long-Term Effects: After frostbite, you might have lasting changes in sensation, tingling, increased sweating, or even bone problems like arthritis in the affected area.
Grades of Recovery
Doctors use a grading system to predict how well someone will recover:
- Grade 1: If there's no initial damage, full recovery is expected.
- Grade 2: If the outer part of a limb is damaged, tissue and fingernails might be destroyed.
- Grade 3: If the middle part of a limb is damaged, the affected part might fall off, and you could lose some function.
- Grade 4: If the injury is very close to the body (like the bones in the hand), the entire limb might be lost. Serious body-wide infections can also occur.
History of Frostbite
Frostbite has been a problem for people for thousands of years.
- The ancient Greeks knew about frostbite around 400 BC.
- Evidence of frostbite was found on a 5,000-year-old mummy from the Andes mountains.
- During Napoleon's invasion of Russia in the early 1800s, many soldiers suffered from cold injuries.
- It's estimated that nearly a million soldiers got frostbite in the First and Second World Wars and the Korean War.
Famous Cases of Frostbite
Several famous people have suffered from frostbite:
- Captain Lawrence Oates: An English explorer who died from frostbite complications in Antarctica in 1912.
- Harold Bride: The junior wireless operator on the RMS Titanic. He got severe frostbite on his feet after standing in freezing water for a long time on a capsized lifeboat.
- Hugh Herr: A well-known American rock climber who lost both legs below the knee to frostbite in 1982 after being stuck in a blizzard on Mount Washington.
- Beck Weathers: A survivor of the 1996 Mount Everest disaster who lost his nose and hands to frostbite.
- Jamie Andrew: A Scottish mountaineer who had all four limbs amputated in 1999 due to severe frostbite after being trapped for four nights while climbing in the Mont Blanc massif.
See also
 In Spanish: Congelamiento para niños
In Spanish: Congelamiento para niños

