Artificial cardiac pacemaker facts for kids
Quick facts for kids Artificial cardiac pacemaker |
|
|---|---|

St. Jude single-lead pacemaker with ruler in cm (released in 2005)
|
|
| Specialty | Cardiology, electrophysiology |
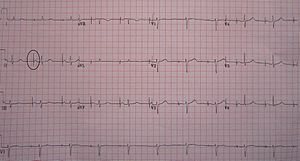
An artificial cardiac pacemaker (often just called a pacemaker) is a small medical device. Doctors put it inside a person's body. It sends out tiny electrical pulses to the heart. These pulses help the heart beat at the right speed and rhythm.
The heart has four main chambers: two upper ones called atria and two lower ones called ventricles. The pacemaker sends signals to one or more of these chambers. Each pulse makes the heart chamber contract (squeeze). This helps the heart pump blood around the body properly.
Pacemakers are mainly used when a person's natural heart rhythm is too slow. This can happen if the heart's own "natural pacemaker" isn't working well. Or, it can be due to a heart block, which means electrical signals in the heart get stuck. Modern pacemakers can be adjusted by doctors from outside the body. This lets them choose the best way for the pacemaker to work for each patient. Most pacemakers only send a pulse when needed. This means they only work if the heart's natural beat is too slow. Some pacemakers send out pulses at a steady rate.
There are also special types of pacemakers. An implantable cardioverter-defibrillator (ICD) can act as both a pacemaker and a defibrillator. This means it can help the heart beat normally and also deliver a stronger shock if the heart beats dangerously fast. Other pacemakers, called biventricular pacemakers, have more wires. They help the lower heart chambers (ventricles) beat together more effectively.
How Do Doctors Pace the Heart?
Doctors can use different methods to help the heart beat. Some are for emergencies, and others are for long-term use.
Emergency Pacing Methods
Sometimes, doctors need to help a heart beat right away in an emergency.
Chest Thumping (Percussive Pacing)
This is a very old and rare emergency method. A doctor might hit the lower part of the chest with their fist. This can sometimes create a small electrical signal to make the heart beat. It's only used until an electrical pacemaker can be brought to the patient.
External Pacing (Transcutaneous Pacing)
For this method, doctors place two special pads on the patient's chest. These pads send electrical pulses through the skin to the heart. Doctors can adjust how fast the pulses are sent. This method is used for a short time in emergencies. It helps keep the heart beating until a more stable solution can be found.
Temporary Pacing During Surgery (Epicardial Pacing)
During open heart surgery, the heart's electrical system can sometimes be affected. Doctors might place small wires directly on the outside surface of the heart (the epicardium). These wires are connected to an external pacemaker. This helps the heart keep pumping well during and after the surgery.
Temporary Pacing Through a Vein (Transvenous Pacing)
This method is also for temporary use. A thin wire is carefully placed into a vein, usually in the neck or groin. The wire is then guided into the heart's upper or lower chamber. This wire connects to a pacemaker device outside the body. This temporary pacemaker can be used until a permanent one is ready. Or, it can be removed if the heart no longer needs help.
Permanent Pacemakers
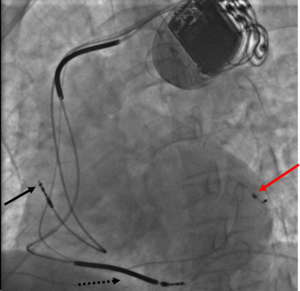
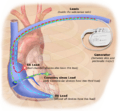
A permanent pacemaker is a device that stays inside the body. Doctors place one or more wires (called leads) into the heart's chambers. The main part of the pacemaker, called the generator, is placed under the skin. It's usually put below the collarbone.
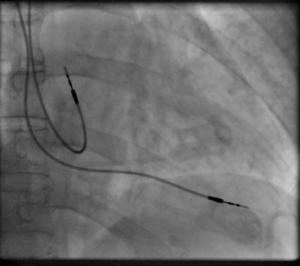
To put it in, a doctor makes a small cut. They guide the lead through a vein and into the heart. They use X-ray images to see where the lead is going. Once the lead is in the right spot, it's connected to the pacemaker generator. The generator is then placed under the skin, and the cut is closed.
There are a few main types of permanent pacemakers:
- Single-chamber pacemaker: This type has one lead. It's placed in either the upper chamber (atrium) or a lower chamber (ventricle) of the heart.
- Dual-chamber pacemaker: This has two leads. One lead goes to an atrium, and the other goes to a ventricle. This helps the upper and lower chambers work together, much like a healthy heart.
- Biventricular pacemaker: This pacemaker has three leads. One is in an atrium, and two are in the ventricles. It's more complex to put in.
- Rate-responsive pacemaker: This smart pacemaker has sensors. It can tell when you are active, like running or playing. It then automatically speeds up or slows down your heart rate to match your body's needs.
The pacemaker generator is a sealed box. It holds a battery (usually a lithium battery). It also has a tiny computer that senses your heart's natural beats. If your heart doesn't beat on its own, the computer sends an electrical pulse. The outside of the pacemaker is usually made of titanium. This metal is safe for the body and rarely causes problems.
Tiny Pacemakers Without Leads (Leadless Pacing)
Newer pacemakers are very small, about the size of a vitamin capsule. These "leadless" pacemakers are placed directly inside the heart. Doctors insert them using a thin tube (catheter) through a vein in the leg. Since they don't have leads, they avoid problems that can happen with wires over time.
How Pacemakers Work
Modern pacemakers have many features. The most basic job is to listen to your heart's natural rhythm. If the pacemaker doesn't hear a natural beat within a certain time (like one second), it sends a small electrical pulse. This pulse makes the heart chamber contract. If the pacemaker does sense a natural beat, it waits. This "demand pacing" happens beat by beat.
In a dual-chamber pacemaker, if the upper chambers beat, the device waits a short time for the lower chambers to beat. If they don't, it sends a pulse to make them beat. This helps keep the heart's chambers working in sync.
Some pacemakers are designed to let your heart's natural rhythm take over if it becomes normal. They will only start helping again if your heart's rhythm becomes a problem.
Biventricular Pacing for Heart Failure
Cardiac resynchronization therapy (CRT) is a special type of pacing. It's used for people with heart failure whose heart chambers don't squeeze at the same time. A biventricular pacemaker (BVP) is used for CRT. It paces both sides of the left ventricle (the main pumping chamber). This helps the ventricles squeeze together, making the heart pump blood more effectively.
CRT devices usually have at least two leads, sometimes three. They help coordinate the timing between the upper and lower heart chambers. They also help the left ventricle's walls squeeze together. CRT can make people with heart failure feel better and live longer.
Some CRT devices also include a defibrillator function. These are called CRT-D devices. They can deliver a shock to stop dangerous fast heart rhythms.
Pacing the Heart's Natural Wires
Doctors are also exploring new ways to place pacemaker leads. Instead of just pacing the tip of the right ventricle, they can try to stimulate the heart's natural electrical wiring system. This is called His bundle pacing. It helps the heart beat in a more natural and effective way. This can prevent long-term problems with the heart muscle.
Smart Pacemakers
A big step forward in pacemakers is making them "rate-responsive." These pacemakers try to copy how a natural heart works. They use sensors to detect things like your physical activity, body temperature, or even oxygen levels. This allows the pacemaker to adjust your heart rate. So, if you start exercising, the pacemaker can make your heart beat faster. If you rest, it can slow it down. The first dynamic pacemaker was invented in London in 1982.
Many modern pacemakers are controlled by tiny computers. These "dual-chamber" pacemakers can control both the upper and lower heart chambers. This helps the heart pump blood more efficiently.
Newer devices can also reduce how much they pace the right ventricle. This is important because too much pacing there can sometimes make heart failure worse.
Living with a Pacemaker
Getting a Pacemaker
Having a pacemaker put in is usually a quick surgery. You might be awake with medicine to numb the area, or you might be asleep. Doctors give antibiotics to prevent infection. The pacemaker is usually placed under the skin near your shoulder. A small cut is made, and a space is created for the pacemaker generator. The wires are guided into your heart using X-ray images. The surgery usually takes 30 to 90 minutes.
After surgery, you need to keep the cut clean and dry. For a few weeks, you might need to limit some shoulder movements. This helps the pacemaker wires settle in place.
The battery in a pacemaker usually lasts 5 to 10 years. When the battery gets low, the doctor replaces only the generator. This is a simpler surgery than the first one.
Regular Checkups
After getting a pacemaker, you'll have regular checkups. These are usually every six months. Doctors check if the device is working well. They can also check it remotely from your home using a special device.
During a checkup, doctors look at:
- If the pacemaker can "see" your heart's natural beats.
- The condition of the wires.
- How much power is needed to make your heart beat.
- How often the pacemaker has been working.
- How much battery life is left.
- Any unusual heart rhythms the pacemaker has recorded.
Everyday Life with a Pacemaker
Most people with a pacemaker can live a normal life. You should avoid full-contact sports. Also, keep the pacemaker away from very strong magnetic fields.
Some everyday things might need small adjustments. For example, a car seatbelt might feel uncomfortable over the pacemaker. Special protection can be worn for some sports.
Magnets and Other Devices
Strong magnetic or electromagnetic fields can sometimes affect pacemakers. However, most household items are safe. It's best to keep objects with strong magnets away from your pacemaker. This includes some headphones or induction cooktops.
Many modern pacemakers are now "MRI conditional." This means they are safe to use during an MRI scan, but only under specific conditions set by the doctor. If you have an older pacemaker, an MRI might not be safe.
Always tell doctors, dentists, and other medical staff that you have a pacemaker before any procedure.
Patient Choices and Pacemakers
Patients, or their families, have the right to make decisions about their medical care. This includes decisions about a pacemaker. If a patient has a serious illness and decides they no longer want the pacemaker to help them, they can discuss this with their doctor. Doctors will help patients understand their choices and support their decisions.
Possible Problems
Problems from pacemaker surgery are rare (about 1-3%). They can include:
- Infection where the pacemaker is placed.
- An allergic reaction to medicines used during surgery.
- Swelling, bruising, or bleeding around the pacemaker.
Sometimes, the pacemaker wires (leads) can move out of place or wear out over time. If this happens, they might need to be adjusted or replaced. Replacing leads can be more complex than replacing the generator.
Overall, people with pacemakers usually have a very good life expectancy. It mostly depends on their other health conditions.
Other Heart Devices
Sometimes, devices similar to pacemakers, called implantable cardioverter-defibrillators (ICDs), are implanted. These devices are used for people at risk of sudden serious heart problems. An ICD can do many things: it can pace the heart, or it can deliver an electrical shock (called cardioversion or defibrillation) to fix very fast or irregular heart rhythms. Some ICDs can even try to speed up the heart to break a fast rhythm before it becomes dangerous.
History of Pacemakers
The idea of using electricity to make the heart beat goes back a long way.
Early Ideas
In 1889, a scientist named John Alexander MacWilliam showed that electrical pulses could make a heart beat. In 1926, Dr. Mark C. Lidwill and physicist Edgar H. Booth in Australia created a portable device. It could send electrical pulses to the heart. In 1928, they used it to help a newborn baby whose heart wasn't beating.
In 1932, American physiologist Albert Hyman built his own electrical device. He was the first to call it an "artificial pacemaker." For a while, people were not very open to the idea of "interfering with nature" by restarting hearts.
External Pacemakers
In 1950, Canadian engineer John Hopps built the first external pacemaker. It was a large device that plugged into a wall socket. It was a bit uncomfortable and could be risky.
Later, in 1952, Paul Zoll made smaller, battery-powered external pacemakers. In 1958, engineer Earl Bakken made the first wearable external pacemaker. It was a small box that patients could wear. Wires from the box went through the skin to the heart.
First Implantable Pacemakers
The first time a fully implantable pacemaker was put into a human was on October 8, 1958, in Sweden. It was designed by Rune Elmqvist and Åke Senning. This first device only worked for three hours. A second one lasted two days. The patient, Arne Larsson, lived a long life and had 26 different pacemakers over the years!
In 1959, doctors found a way to put temporary pacemaker wires into a vein. This was less invasive than surgery.
In February 1960, an improved Swedish pacemaker was implanted in Uruguay. It worked for nine months until the patient died from other health issues.
Engineer Wilson Greatbatch created implantable pacemakers that used batteries. These were first used in humans in April 1960. The first patient lived for 18 more months.
By the mid-1960s, putting pacemaker wires through a vein became the most common method.
Better Batteries and Design
Early pacemakers had batteries that didn't last long. In the late 1960s, some companies tried using atomic batteries, but this didn't become common.
A big change happened in 1971 with the invention of the lithium iodide battery. This battery made pacemakers last much longer, from one year to up to eleven years. Lithium batteries are still used today.
Another improvement was making the pacemaker generator sealed in a metal case, usually titanium. This protected the electronics from body fluids and made pacemakers more reliable. This became standard by the mid-1970s.
Modern Tiny Pacemakers
In 2013, companies started making very small pacemakers. These are about the size of a pill and can be inserted through a leg vein. They don't need wires. These tiny devices are still being developed and tested.
Reusing Pacemakers
Every year, thousands of pacemakers are removed from bodies before cremation. Many of these devices still have good battery life. Some people believe these pacemakers could be safely cleaned and reused for patients in poorer countries. This could save lives, but there are still legal and safety challenges to make this a common practice.
Pacemaker Makers
Here are some companies that make or used to make implantable pacemakers:
- Biotronik (Germany)
- Boston Scientific (USA)
- Cardiac Pacemaker Inc. ; Guidant (USA) (now part of Boston Scientific)
- Intermedics (USA)
- Lepu Medical (China)
- Medico (Italy)
- Medtronic (USA)
- Sorin Group (Italy) (now part of LivaNova; its pacemaker business was sold to MicroPort)
- St. Jude Medical (USA) (now part of Abbott Laboratories)
- Abbott (USA)
See Also
 In Spanish: Marcapasos cardíaco artificial para niños
In Spanish: Marcapasos cardíaco artificial para niños
- Biological pacemaker
- Button cell
- Electrical conduction system of the heart
- Implantable cardioverter-defibrillator
- Infective endocarditis
- Pacemaker syndrome
Images for kids