Artificial heart facts for kids
Quick facts for kids Artificial heart |
|
|---|---|

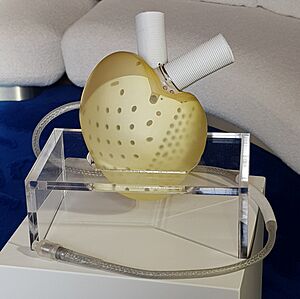
The CardioWest (now SynCardia) Temporary Total Artificial Heart
|
|
| Specialty | {{#statements:P1995}} |
An artificial heart is a special device that can take the place of a human heart. Doctors use artificial hearts mainly to help patients who are waiting for a heart transplant. This gives them more time until a donor heart becomes available. Scientists are also working to create artificial hearts that could stay in a person permanently. This would be for people who cannot get a transplant.
As of December 2023, there are two types of full artificial hearts that doctors can use. Both are for temporary use, usually for less than a year. They help patients with serious heart failure who are waiting for a human heart transplant.
The first artificial heart successfully put into a human was the Jarvik-7 in 1982. It was designed by a team including Willem Johan Kolff, William DeVries, and Robert Jarvik.
An artificial heart is different from a ventricular assist device (VAD). A VAD helps a failing heart pump blood but does not replace it completely. It is also different from a cardiopulmonary bypass machine. This machine is used outside the body during surgery to do the work of both the heart and lungs for a few hours.
Contents
Understanding Artificial Hearts
What is an Artificial Heart?
Imagine your heart as a powerful pump that sends blood all over your body. An artificial heart is a machine designed to do this job when your own heart can no longer work. It's like a replacement pump.
Scientists have been trying to create a working artificial heart for a long time. It's a big challenge because the human heart is very complex. It needs to pump blood just right, and the materials used in an artificial heart must be safe for the body. They also need to last a long time.
Early artificial hearts faced problems like blood clots forming or the body rejecting the device. But medical technology keeps getting better. Newer artificial hearts are designed to reduce these problems.
Early Steps in Heart Support
The idea of replacing a heart started many years ago.
- In 1938, a Soviet scientist named Vladimir Demikhov made the first artificial heart. He put it into a dog.
- In 1952, doctors used a machine called the Dodrill-GMR heart machine during heart surgery. It helped a patient's heart for 50 minutes. This was a big step forward.
- In 1953, the first heart-lung machine was used successfully during open heart surgery. This machine temporarily takes over for the heart and lungs.
These early successes showed that it was possible to support the body when the heart wasn't working. This led many scientists to try and develop a full artificial heart.
Designing the First Artificial Hearts
Many different designs for artificial hearts were tried over the years.
- In 1949, doctors William Sewell and William Glenn built an early heart pump using simple toys and parts. It worked for over an hour in a dog.
- In 1957, Willem Johan Kolff, a famous inventor of artificial organs, put an artificial heart into a dog. The dog lived for 90 minutes.
- In 1958, Domingo Liotta began studying total artificial hearts in France and Argentina. He showed his work in 1961.
- In 1961, Paul Winchell (a famous ventriloquist!) designed an artificial heart model. He worked with Henry Heimlich, who invented the Heimlich maneuver.
- In 1964, the National Institutes of Health started a program to develop an implantable artificial heart. They wanted to put one into a human by the end of the decade.
- In 1966, Adrian Kantrowitz performed the world's first permanent implant of a partial mechanical heart. This was a device that helped the heart's lower left chamber.
The Jarvik Hearts Story
In 1967, Dr. Kolff moved to the University of Utah to continue his work on artificial hearts. Many people helped him, including a student named Robert Jarvik. The "Jarvik" line of artificial hearts is named after him.
- In 1973, a calf named Tony lived for 30 days with an early Kolff heart.
- In 1975, a bull named Burk lived for 90 days.
- In 1976, a calf named Abebe lived for 184 days with the Jarvik 5 heart.
- In 1981, a calf named Alfred Lord Tennyson lived for 268 days with the Jarvik 5.
Robert Jarvik made important improvements to the design. He made the heart an oval shape to fit better in the human chest. He also used a special material that was safer for blood. This helped reduce dangerous blood clots.
First Human Implants
The first time a mechanical heart was put inside a person's chest as a temporary bridge to a transplant was on April 4, 1969. Domingo Liotta and Denton Cooley did this surgery in Houston, Texas. The patient started to recover, and after 64 hours, the artificial heart was removed and replaced with a donor heart. Sadly, the patient died later from an infection.
The first time an artificial heart was used for a long-term replacement, not just a bridge to transplant, was in 1982.
- On December 1, 1982, Dr. William DeVries implanted the Jarvik-7 artificial heart into Barney Clark. He was a retired dentist with severe heart failure.
- Barney Clark's case was very famous and got a lot of media attention. He lived for 112 days with the artificial heart. It was connected to a large machine that weighed about 400 pounds.
- Even with some difficulties, Clark felt he was helping medicine. He died on March 23, 1983.
Dr. DeVries continued his work with the Jarvik-7.
- His next patient was Bill Schroeder, who received the Jarvik-7 on November 25, 1984. Schroeder lived for 620 days with the artificial heart. He even got to use a portable battery-powered device that let him leave the hospital for short times.
- Other patients also received the Jarvik-7. While they faced challenges, their experiences helped doctors learn a lot about artificial hearts.
These early artificial hearts needed large machines to power them. Two tubes also had to go through the patient's skin to connect to the heart. This increased the risk of infection. Scientists then started working on smaller, electrically powered artificial hearts.
Helping a Failing Heart
Sometimes, a device is used to help a failing heart, rather than replacing it completely.
- In 1963, the first Left Ventricular Assist Device (LVAD) was implanted. This device helps the left side of the heart pump blood.
- In 1966, Michael E. DeBakey and Liotta implanted an LVAD that rested outside the patient's body. One patient recovered well and went home after 10 days.
- In 1990, Brian Williams became the first VAD patient to go home from the hospital with FDA approval.
Modern Artificial Hearts
SynCardia Artificial Heart
SynCardia Systems makes two models of their artificial heart. One is for adult men, and a smaller one is for children and women. By 2014, over 1,250 patients had received SynCardia artificial hearts.
The device has two power systems. One is for use in the hospital. The other is a portable system called the Freedom Driver System. This allows some patients to go home. These systems send air pulses to the heart through tubes. They also check blood flow.
The SynCardia heart is based on the Jarvik-7 design. But it has been improved over time. These improvements have reduced problems like strokes and bleeding. Patients have also lived much longer with the device. One patient lived for over 1,700 days (more than 4.5 years!).
The SynCardia total artificial heart was approved for use in the U.S. in 2004.
Carmat Aeson Bioprosthetic Heart
In 2008, French professor Alain F. Carpentier announced plans for a fully implantable artificial heart. It was developed by his company, CARMAT SA.
- The first Carmat artificial heart was implanted on December 18, 2013, in Paris, France. The patient lived for 75 days.
- The Carmat Aeson heart has two chambers. A pump moves fluid, which makes a membrane move and pump blood.
- The parts that touch the blood are made from animal tissues. This helps the device be more compatible with the body.
- The Carmat heart also has sensors that can adjust blood flow when a patient is exercising.
The Carmat Aeson is meant to be a permanent solution for severe heart failure. It weighs about three times more than a typical human heart. It also needs the patient to carry an external battery pack. The company hopes it will last about 5 years.
In December 2020, the Carmat artificial heart was approved for sale in the European Union. As of December 2023, it is used in Europe as a temporary bridge to transplant. In the United States, it is still being tested in clinical trials.
Other Artificial Heart Ideas
Scientists are always looking for new ways to create artificial hearts.
- The U.S. Army developed a compact, air-powered heart pump in the 1960s.
- The POLVAD system is being developed in Poland. It includes an artificial ventricle and control units. Newer versions are smaller and more mobile.
- The Phoenix-7 Total Artificial Heart was made in Taiwan. In 1996, a patient received this heart and later had a successful combined heart and kidney transplant.
- The AbioCor was implanted in 2001. It was made of titanium and plastic and had an internal battery. Its size made it suitable for only about half of men and less than half of women. The company stopped developing total artificial hearts in 2015.
- In 2011, an experimental artificial heart made of two modified pumps was implanted in a patient in Houston. The patient lived for 5 more weeks.
Future Ideas: Soft and Rotary Hearts
Scientists are exploring new and exciting ideas for artificial hearts.
- Soft Artificial Heart: In 2017, researchers in Switzerland showed a new idea for a soft artificial heart. It's made of silicone and works with pressurized air. It moves and works like a natural heart. The goal is to make it the same size as a real heart. Early versions only worked for a short time, but scientists are working to make them last much longer.
- BiVACOR Artificial Heart: This company is developing an artificial heart that uses a spinning part that floats using magnets. This design aims to reduce blood clots and make the device smaller. It has only one moving part. This heart does not create a pulse like a natural heart, but it can change speed quickly to create "beats." It has been tested in sheep. In November 2023, it was approved for human trials in the U.S.
Helping the Heart: Ventricular Assist Devices (VADs)
Sometimes, a patient's heart still works a little, but not enough. In these cases, doctors might use a Ventricular assist device (VAD). A VAD doesn't replace the whole heart. Instead, it helps the heart by doing much of the pumping work.
- The first LVAD system was created in 1962.
- The Kantrowitz CardioVad can take over more than 50% of the heart's work. For young people, this device might delay the need for a transplant for many years. Sometimes, the heart can even recover, and the VAD can be removed.
- Newer VADs, like the Heartmate II, provide a continuous flow of blood instead of a pulsing flow. These pumps are smaller and can last longer.
- A big advantage of a VAD is that the patient keeps their own heart. If the VAD stops working, the natural heart can still provide some backup.
In 2006, a 15-year-old girl received a Berlin Heart (a type of VAD) in Canada. It was meant to be temporary until she got a donor heart. But the Berlin Heart helped her own heart heal! After 146 days, the device was removed, and her heart worked on its own. The Berlin Heart was approved in the U.S. in 2011 and has helped many children.
Studies have shown that VADs like the Berlin Heart can greatly improve survival for children waiting for heart transplants.
Images for kids
See also
- Organ culture
- Artificial heart valve
- Artificial cardiac pacemaker
- Ventricular assist device