Cancer immunotherapy facts for kids
Quick facts for kids Cancer immunotherapy |
|
|---|---|
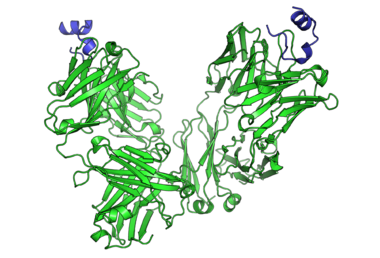
Peptide epitope of CD20 bound to rituximab's FAB
|
|
| Specialty | {{#statements:P1995}} |
Cancer immunotherapy (also called immuno-oncotherapy) is a way to treat cancer. It works by making your body's own immune system stronger. This helps your immune system fight cancer better, using its natural ability to find and destroy sick cells. It's a special part of oncology, which is the study and treatment of cancer.
Cancer immunotherapy uses the fact that cancer cells often have special markers on their surface. These markers are called tumor antigens. Your immune system can learn to spot these markers. Normally, your immune system fights off germs. But with immunotherapy, special treatments help your immune system find and attack cancer cells. The success of this treatment can be different for various types of cancer. Some cancers respond very well, while others do not.
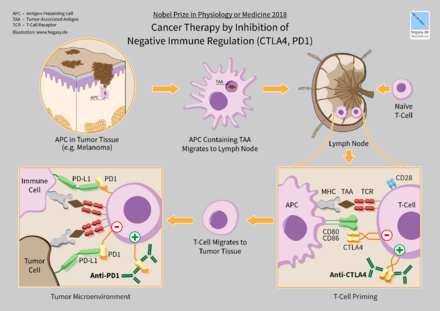
In 2018, two scientists, James P. Allison and Tasuku Honjo, won the Nobel Prize in Physiology or Medicine. They won for finding new ways to treat cancer by helping the immune system.
How Cancer Immunotherapy Started
People have thought about using the immune system to fight cancer for a long time. In the 1700s and 1800s, doctors tried different ways to make the body's defenses work against cancer. They even used infections to help.
A famous story is about an American surgeon named William Coley. In 1891, he noticed that some cancer patients got better after they had a feverish infection. He then tried injecting patients with special heat-killed bacteria. This was to make their immune system react. Coley's method was used for many years, and some patients with serious cancers got much better. His work showed that the immune system could indeed fight cancer.
Different Kinds of Immunotherapy
There are several main types of immunotherapy used to treat cancer today:
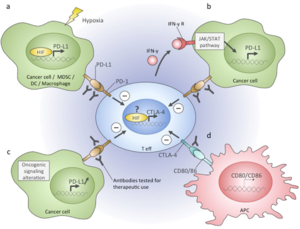
- Immune checkpoint inhibitors: These are medicines that act like releasing the brakes on your immune system. They help your immune cells attack cancer more strongly.
- T-cell transfer therapy: This treatment takes special immune cells called T-cells from a patient's tumor. Scientists then change these cells in the lab to make them better at fighting cancer. After that, the improved T-cells are put back into the patient.
- Monoclonal antibodies: These are like "designer" antibodies. They are made to stick to specific targets on cancer cells. This helps your immune system see and destroy the cancer cells more easily.
- Treatment vaccines: These are not like vaccines for diseases such as the flu. Instead, they help your immune system learn to recognize and destroy cancer cells that have special markers.
- Immune system modulators: These are substances that boost your body's overall immune response against cancer.
Immunotherapies can also be called "active" or "passive." Active immunotherapy directly helps your immune system target cancer cells. Examples include cancer vaccines and special T-cells called CAR-T cells. Passive immunotherapy helps your immune system work better without directly targeting the cancer cells. Examples include checkpoint inhibitors.
Cellular Immunotherapy
This type of immunotherapy uses your own immune cells to fight cancer.
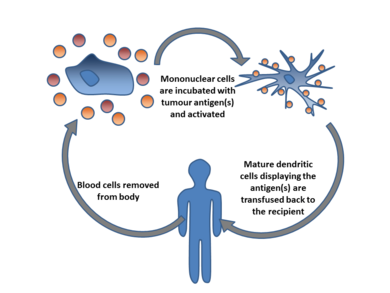
Dendritic Cell Therapy
Dendritic cells are special immune cells that act like messengers. They show other immune cells what to attack. In this therapy, doctors take dendritic cells from a patient. They then teach these cells to recognize cancer markers outside the body. After that, the "trained" dendritic cells are put back into the patient. This helps the immune system find and kill cancer cells.
One way to do this is by mixing the dendritic cells with parts of the patient's own cancer cells. This teaches the dendritic cells what the cancer looks like. Sometimes, other substances are added to make the immune response even stronger.
Adoptive T-cell Therapy
This therapy involves taking T-cells from a patient and making them stronger to fight cancer. T-cells are a type of white blood cell that can find and destroy sick cells.
Doctors can get T-cells from a tumor itself or from the patient's blood. These T-cells can then be changed in different ways. They can be grown in large numbers in the lab. Then, these powerful T-cells are put back into the patient. They are now ready to attack the cancer.
CAR-T Cell Therapy
CAR-T cell therapy is a very special type of T-cell therapy. Scientists take a patient's T-cells and change them genetically. They add a new part called a "chimeric antigen receptor" (CAR). This CAR helps the T-cells specifically recognize and destroy cancer cells.
For example, a CAR-T therapy called Tisagenlecleucel (Kymriah) was approved in 2017. It treats a type of blood cancer called acute lymphoblastic leukemia (ALL). Another one, Axicabtagene ciloleucel (Yescarta), was approved for a type of lymphoma.
Multifunctional Alginate Scaffolds (MASTER)
MASTER is a new way to make CAR-T cells inside the body. Instead of taking weeks, this method takes only hours. T-cells are mixed with a special virus that helps them become CAR-T cells. This mixture is then put into a special "scaffold" (like a tiny sponge). This scaffold is placed inside the patient. The T-cells become CAR-T cells and multiply, then leave the scaffold to fight the cancer. This method might make the treatment stronger and last longer.
Antibody Therapy
Antibody therapy uses special proteins called antibodies. These antibodies are designed to find and stick to specific targets on cancer cells. When they stick, they can help the immune system destroy the cancer cells.
Types of Antibodies
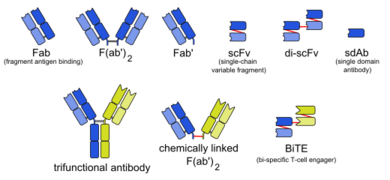
Antibodies used in cancer treatment can be:
- Naked monoclonal antibodies: These are just the antibodies themselves, without anything extra attached. Most antibody therapies use this type.
- Conjugated monoclonal antibodies: These antibodies have another molecule attached to them. This extra molecule can be a strong chemical or something radioactive. The antibody acts like a guide, taking the toxic substance directly to the cancer cells.
Antibodies can also come from different sources. Some are made from human cells, some from mice, and some are a mix of both. Human antibodies are usually best because the patient's body is less likely to react against them.
How Antibodies Work
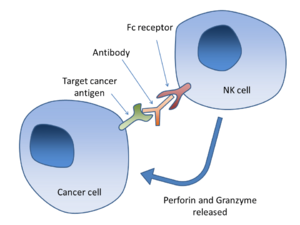
One way antibodies work is called Antibody-dependent cell-mediated cytotoxicity (ADCC). Imagine an antibody sticking to a cancer cell. This antibody has a special "tail" (called the Fc region). Certain immune cells, like NK cells, have "receptors" that can grab onto this tail. When an NK cell grabs onto the antibody, it releases chemicals that kill the cancer cell.
Another way is by blocking certain proteins. Some antibodies block proteins that normally tell the immune system to slow down. By blocking these "brakes," the antibodies allow the immune system to attack the tumor more strongly.
Anti-CD47 Therapy
Many cancer cells have a protein called CD47 on their surface. This protein acts like a "don't eat me" signal to immune cells. Anti-CD47 therapy uses antibodies to block this signal. This allows immune cells to "eat" and destroy the cancer cells.
Anti-GD2 Antibodies
Some cancer cells have a sugar molecule called GD2 on their surface. This molecule is usually not found on healthy cells. This makes GD2 a good target for immunotherapy. Antibodies can be designed to specifically attack cells that have GD2. This type of therapy is being studied for many different cancers, including neuroblastoma and melanoma.
FDA-Approved Antibodies
Many antibody drugs have been approved by the FDA (Food and Drug Administration) to treat different cancers. Here are a few examples:
| Antibody | Brand name | Type | Target | Approval date | Approved treatment(s) |
|---|---|---|---|---|---|
| Alemtuzumab | Campath | humanized | CD52 | 2001 | B-cell chronic lymphocytic leukemia (CLL) |
| Atezolizumab | Tecentriq | humanized | PD-L1 | 2016 | bladder cancer |
| Avelumab | Bavencio | human | PD-L1 | 2017 | metastatic Merkel cell carcinoma |
| Ipilimumab | Yervoy | human | CTLA4 | 2011 | metastatic melanoma |
| Elotuzumab | Empliciti | humanized | SLAMF7 | 2015 | multiple myeloma |
| Ofatumumab | Arzerra | human | CD20 | 2009 | refractory CLL |
| Nivolumab | Opdivo | human | PD-1 | 2014 | unresectable or metastatic melanoma, squamous non-small cell lung cancer, Renal cell carcinoma, colorectal cancer, hepatocellular carcinoma, classical hodgkin lymphoma |
| Pembrolizumab | Keytruda | humanized | PD-1 | 2014 | unresectable or metastatic melanoma, squamous non-small cell lung cancer (NSCLC), Hodgkin's lymphoma, Merkel-cell carcinoma (MCC), primary mediastinal B-cell lymphoma (PMBCL), stomach cancer, cervical cancer |
| Rituximab | Rituxan, Mabthera | chimeric | CD20 | 1997 | non-Hodgkin lymphoma |
| Durvalumab | Imfinzi | human | PD-L1 | 2017 | bladder cancer non-small cell lung cancer |
Ipilimumab
Ipilimumab (Yervoy) is an antibody that blocks a protein called CTLA4. CTLA4 acts like a "brake" on T-cells, slowing them down. By blocking CTLA4, ipilimumab helps T-cells become more active and attack melanoma cells.
Nivolumab
Nivolumab (Opdivo) is an antibody that blocks another "brake" protein called PD-1. Cancer cells sometimes use PD-1 to hide from T-cells. By blocking PD-1, nivolumab allows T-cells to see and attack the cancer. It's used for several cancers, including melanoma and lung cancer.
Pembrolizumab
Pembrolizumab (Keytruda) is another PD-1 blocker, similar to nivolumab. It helps T-cells fight cancer by removing the "brake" on their activity. It is used for melanoma, lung cancer, Hodgkin's lymphoma, and other cancers.
Rituximab
Rituximab (Rituxan) is an antibody that targets a protein called CD20. CD20 is found on certain immune cells called B-cells, including cancerous B-cells in some lymphomas and leukemias. When rituximab binds to CD20, it helps the immune system destroy these cancer cells.
Immune Checkpoint Blockade
Immune checkpoints are like switches that control the immune system. Some checkpoints turn the immune system "on," and others turn it "off." Cancer cells can sometimes use the "off" switches to protect themselves from being attacked by the immune system.
Immune checkpoint blockade therapies work by blocking these "off" switches. This allows the immune system to become more active and fight the tumor. While these therapies can be very effective for some cancers, like Hodgkin lymphoma, they don't work for everyone. Scientists are still trying to understand why.
One important "off" switch involves two proteins: PD-1 and PD-L1. PD-L1 is often found on cancer cells, and it binds to PD-1 on immune cells. This binding tells the immune cell to stop attacking. Antibodies that block either PD-1 or PD-L1 can stop this signal, allowing the immune cells to attack the tumor.
Combining Therapies
Many patients don't respond to just one type of immune checkpoint blockade. Doctors are finding that combining these therapies with other treatments can improve results. For example, combining different checkpoint inhibitors or adding other drugs can make the immune system even stronger against cancer.
Cytokine Therapy
Cytokines are proteins that act as messengers between immune cells. They help control how the immune system responds. Sometimes, tumors use cytokines to grow and hide from the immune system. But doctors can also use cytokines as medicines to boost the immune response against cancer.
Two common cytokines used in treatment are interferons and interleukins.
- Interferon-α is used for some types of leukemia and melanoma.
- Interleukin-2 is used for melanoma and kidney cancer.
These cytokines help the immune system become more active and fight the tumor.
Genetic Testing for Treatment
Before starting immunotherapy, doctors sometimes do genetic tests. These tests look for specific changes in the cancer cells' DNA. These changes can help predict if a patient will respond well to certain immunotherapy drugs.
For example, tests can look for the amount of "mutations" (changes) in the cancer's DNA. Cancers with more mutations might respond better to immunotherapy. However, this area is still being researched, and not all tests are perfect.
New Research in Immunotherapy
Scientists are always looking for new ways to use the immune system to fight cancer.
Oncolytic Viruses
An oncolytic virus is a special type of virus that can infect and kill cancer cells. When the virus destroys cancer cells, it also releases new virus particles to attack more tumor cells. These viruses also help to kick-start the body's immune system to fight the tumor in the long term.
One oncolytic virus, T-Vec, has been approved for treating melanoma. Many other oncolytic viruses are being studied in clinical trials.
Medicinal Mushrooms
Some compounds found in mushrooms, especially certain polysaccharides, can boost the immune system. These compounds, like beta-glucans, have been shown in lab studies to activate immune cells. They are being studied to see if they can help in cancer treatment. In Japan, a mushroom extract called polysaccharide-K is approved to help patients undergoing chemotherapy.
Neoantigens
Many tumors have unique changes called "neoantigens." These are like new flags on the cancer cells that the immune system might not recognize at first. Scientists are studying how to use these neoantigens to create even more targeted T-cell immunotherapies. Cancers with more of these unique changes often respond better to immunotherapy.
See also
- Cancer vaccine
- Coley's toxins
- Cryoimmunotherapy
- Photoimmunotherapy
- Radioimmunotherapy
 | Dorothy Vaughan |
 | Charles Henry Turner |
 | Hildrus Poindexter |
 | Henry Cecil McBay |