Heart transplantation facts for kids
A heart transplant is a special surgery. Doctors replace a very sick heart with a healthy one from a donor. This surgery is for people whose hearts are failing and other treatments haven't worked. It gives them a chance to live longer and feel better.
Most often, the new heart comes from someone who has recently passed away. Doctors carefully place this new heart into the patient's chest. Sometimes, the patient's own heart is removed. In rarer cases, the sick heart is left in place to help the new heart.
Around 5,000 heart transplants happen worldwide each year. More than half of these are in the United States. After the surgery, many patients live for about 15 more years. A heart transplant isn't a "cure" for heart disease. Instead, it's a life-saving treatment that greatly improves a person's life.
Heart Transplants: A New Chance for Life
A Look Back: The History of Heart Transplants
Early Ideas and Experiments
In 1907, a researcher named Simon Flexner imagined that one day doctors might replace sick organs, including the heart. This was a very bold idea at the time!
In 1964, Dr. James D. Hardy tried an experimental transplant. He used a chimpanzee heart for a very ill patient. The heart beat for a short time, but the patient did not recover. This early attempt helped doctors learn more about transplants.
Later, in January 2022, a major step happened. Surgeon Bartley P. Griffith performed the world's first successful transplant of a pig's heart into a human. The pig's heart was specially modified for this. The patient, David Bennett, lived for two months after this groundbreaking surgery.
First Human Transplants
The first human-to-human heart transplant was on December 3, 1967. Dr. Christiaan Barnard in South Africa performed it. The patient, Louis Washkansky, lived for 18 days but then passed away from pneumonia.
Just a few days later, on December 6, 1967, Dr. Adrian Kantrowitz did the first heart transplant for a child in New York. The new heart stopped beating after 7 hours.
In January 1968, Dr. Norman Shumway did the first adult heart transplant in the United States. Soon after, Dr. Donald Ross performed the first in the United Kingdom. These were all allotransplants, meaning the heart came from another human.
Many doctors tried over 100 transplants in 1968. But only about a third of these patients lived longer than three months.
Important Discoveries and Progress
A big improvement came in 1983 with a medicine called cyclosporine. This drug helped stop the body from rejecting the new heart. It made transplants much safer and more successful.
In 1984, JP Lovette IV, a 4-year-old boy, had the world's first successful heart transplant for a child. He was born with several heart problems.
In 1988, doctors performed the first "domino" heart transplant. This is when a patient needing a lung transplant gets a new heart and lungs. Their healthy original heart is then given to another patient.
Today, about 5,000 heart transplants happen each year. This number has grown a lot in recent years. Most of these surgeries take place in the United States.
Because many people need new hearts, scientists are also researching other options. These include using hearts from other animals (called xenografts) or creating artificial hearts.
Medical teams around the world continue to perform more transplants. For example, Sri Lanka had its first heart transplant in 2017.
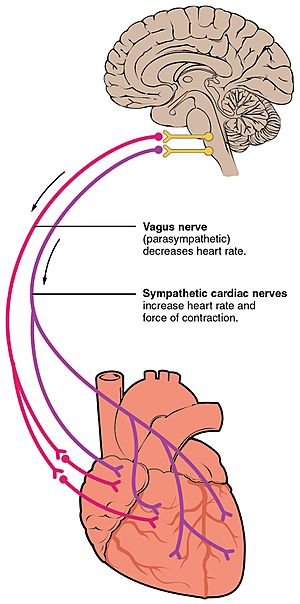
During a heart transplant, some nerves to the heart are cut. This means the brain's direct control over the new heart changes. However, some nerve connections can slowly return over time.
Recently, researchers in Australia found ways to keep donor hearts healthy for longer before surgery. This gives doctors more time for the transplant.
Doctors are also using hearts from donors after their circulation has stopped (called DCD). This helps more people get transplants and reduces waiting times.
In April 2023, surgeons at Stanford Medicine performed the first transplants using beating hearts from donors after circulatory death.
When a Heart Transplant Might Not Be Possible
Not everyone can have a heart transplant. Doctors check for other health problems that could make the surgery too risky or prevent a good recovery. These are called contraindications.
Absolute Contraindications
These are conditions that almost always prevent a transplant:
- Serious, lasting problems with other organs like the kidneys, lungs, or liver.
- Active cancer that could make the transplant unsafe or shorten the patient's life.
- Other serious illnesses or infections not related to the heart problem.
- Problems with blood vessels in other parts of the body, like the neck or legs.
- Very high pressure in the blood vessels of the lungs.
Relative Contraindications
These conditions might make a transplant more difficult, and doctors decide based on each patient:
- Severe diabetes that has affected other organs.
- A recent serious blood clot, like a stroke.
- Very high weight (severe obesity).
- Being over a certain age, often around 65, though doctors look at each person individually.
- Habits that could harm the new heart or make recovery difficult, like smoking.
If a patient can't have a heart transplant, doctors might suggest other devices. These include an artificial heart or a special pump called a left ventricular assist device (LVAD).
What Can Happen After a Transplant?
Like any major surgery, heart transplants can have problems, called complications. Doctors work hard to prevent these.
Some risks right after surgery include infections. About 5-10% of patients faced serious complications from the surgery itself in 2011.
The body's immune system might try to reject the new heart. This is a major concern.
Other problems can include issues with the new heart's blood vessels, irregular heartbeats, or problems with one of the heart valves. Patients also have a higher risk of certain types of cancer or other infections because of the medicines they take.
Doctors often take small samples of the new heart (a biopsy) to check for rejection. This test can sometimes cause minor issues like bleeding.
Understanding Rejection
When a new heart is placed in the body, the patient's immune system sees it as 'foreign.' It tries to attack and reject the new heart. This happens even if the donor heart is a good match.
To stop rejection, patients must take special medicines called immunosuppressants for the rest of their lives. These medicines weaken the immune system. While they are vital, they can have side effects. For example, they can make patients more likely to get infections or develop certain types of cancer. They can also sometimes affect the kidneys.
Scientists are always looking for better ways to prevent rejection and reduce medicine side effects. Research, often using studies with animals like mice, helps find new solutions.
Doctors regularly monitor patients to check for any signs that the body might be rejecting the new heart.
Life After a Heart Transplant
The outlook for people who receive heart transplants has gotten much better. Many people live long and healthy lives after their surgery.
Here are some survival rates for patients who had an orthotopic heart transplant (where the old heart is fully replaced):
- After 1 year: About 88.0% of males and 86.2% of females are still living.
- After 3 years: About 79.3% of males and 77.2% of females are still living.
- After 5 years: About 73.2% of males and 69.0% of females are still living.
See also
 In Spanish: Trasplante de corazón para niños
In Spanish: Trasplante de corazón para niños
- Artificial heart
- Biological pacemaker
- Xenotransplantation
 | William Lucy |
 | Charles Hayes |
 | Cleveland Robinson |