COVID-19 facts for kids
Quick facts for kids Coronavirus disease 2019(COVID-19) |
|
|---|---|
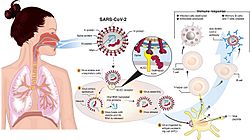
Transmission and life-cycle of SARS-CoV-2, which causes COVID-19
|
|
| Classification and external resources | |
| Synonyms | COVID, (the) coronavirus |
| Specialty | Infectious disease |
| Patient UK | Coronavirus disease 2019 (COVID-19) |
Coronavirus disease 2019 (COVID-19) is a sickness caused by a tiny germ called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This sickness first appeared in Wuhan, China, in December 2019. It quickly spread all over the world, causing a big health crisis called the COVID-19 pandemic.
Contents
What Are the Symptoms?
The symptoms of COVID‑19 can be different for everyone. Common signs include a fever, cough, headache, feeling very tired, and trouble breathing. Some people also lose their sense of smell or taste.
These symptoms can start anywhere from one to fourteen days after someone is exposed to the virus. Interestingly, about one-third of people who get infected don't show any noticeable symptoms at all.
Most people who do get sick have mild to moderate symptoms. This might feel like a bad cold or flu. A smaller number of people get more severe symptoms, needing extra care. Older people are more likely to get very sick.
Some people continue to feel effects for months after getting better. This is sometimes called "long COVID". Scientists are still studying these long-term effects.
How Does COVID-19 Spread?
COVID‑19 spreads when tiny particles with the virus are breathed in. These particles can also get into your eyes, nose, or mouth.
The risk of catching the virus is highest when people are close to each other. However, very small virus particles can stay in the air for a while. They can travel longer distances, especially indoors.
You can also get the virus if you touch a surface or object that has the virus on it, then touch your eyes, nose, or mouth. People can spread the virus for up to 20 days. They can even spread it if they don't feel sick themselves.
What Are the Complications?
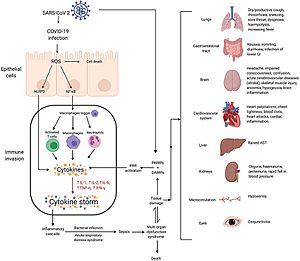
Sometimes, COVID-19 can lead to more serious health problems. These can include pneumonia, which affects the lungs, or problems with the heart. In very serious cases, it can affect many organs in the body.
Children can sometimes develop a rare condition called paediatric multisystem inflammatory syndrome after getting COVID-19. This condition has symptoms similar to Kawasaki disease and can be serious.
Pregnant women might be at a higher risk of getting very sick from COVID-19. This is because the virus can lead to breathing problems or other issues during pregnancy.
What Causes COVID-19?
COVID-19 is caused by a type of coronavirus called 'Severe Acute Respiratory Syndrome coronavirus 2' (SARS-CoV-2). Coronaviruses are a family of viruses that can cause illnesses in humans and animals.
How Can We Prevent It?
There are many ways to help prevent the spread of COVID-19 and protect yourself:
- Get Vaccinated: COVID-19 vaccines are available and help your body fight off the virus. Many countries have given out millions of vaccine doses.
- Stay Home When Sick: If you feel unwell, it's best to stay home to avoid spreading germs.
- Wear a Mask: Wearing a mask in public can help stop the virus from spreading.
- Keep Your Distance: Try to stay a safe distance from others, especially in crowded places.
- Wash Your Hands: Wash your hands often with soap and water for at least 20 seconds. This is a simple but powerful way to remove germs.
- Good Hygiene: Cover your coughs and sneezes. Try not to touch your eyes, nose, or mouth with unwashed hands.
- Ventilate Spaces: Opening windows or using good ventilation indoors can help clear the air.
Effects on Other Diseases
The steps taken to prevent COVID-19, like social distancing and wearing surgical masks, might have had an interesting side effect. They may have also helped reduce the spread of common illnesses like the common cold and the flu.
Images for kids
-
Mechanisms of SARS-CoV-2 cytokine storm and complications
See also
 In Spanish: COVID-19 para niños
In Spanish: COVID-19 para niños
 | Janet Taylor Pickett |
 | Synthia Saint James |
 | Howardena Pindell |
 | Faith Ringgold |