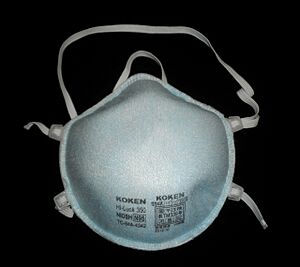
N95 mask facts for kids
An N95 mask or N95 respirator is a special type of respirator that helps filter out tiny particles from the air. It gets its name "N95" because it meets a standard set by the U.S. National Institute for Occupational Safety and Health (NIOSH). This means it can filter at least 95% of airborne particles. Unlike some other masks, N95s are not resistant to oil. They are the most common type of mask that filters particles. These masks protect against small particles, but they don't protect against gases or vapors.
N95 respirators are similar to masks used in other countries, like FFP2 masks in Europe or KN95 masks in China. However, each country has slightly different rules for how these masks are tested and approved.
The N95 mask is made from a very fine mesh of synthetic fibers, often called nonwoven polypropylene fabric. This fabric is created using a special process called melt blowing. This process forms the inner layer that filters out harmful particles from the air.
Contents
How N95 Masks Are Used
In the United States, a group called the Occupational Safety and Health Administration (OSHA) requires healthcare workers to wear N95 respirators. This is especially important when they are caring for patients who might have COVID-19. Unlike an N95 respirator, a surgical mask does not create a tight seal around the face. This means a surgical mask doesn't protect the wearer from tiny airborne particles like viruses.
Getting the Right Fit
Making sure an N95 respirator fits correctly is very important. This is called "fit testing." OSHA requires healthcare workers to have an initial fit test. This test helps find the right model, style, and size of respirator for each person. They also need annual fit tests. Every time someone puts on a tight-fitting respirator like an N95, they must do a "user seal check." This check makes sure the mask is sealed tightly to their face.
Using Masks During Shortages
Sometimes, there aren't enough N95 respirators for everyone who needs them. This happened during the 2019–20 coronavirus pandemic. In such situations, workers should still try to find a respirator that fits them well. Even without a formal fit test, a respirator offers better protection than a surgical mask or no mask at all.
Here are some tips for using N95s during shortages:
- Try different models or sizes to get a good seal on your face.
- Watch videos or read instructions from the manufacturer on how to put on and take off the mask correctly.
- Do a user seal check several times to make sure it's sealed.
- Look in a mirror or ask a friend to check if the mask is touching your face all around.
During the pandemic, the U.S. Centers for Disease Control and Prevention (CDC) suggested ways to use N95 respirators wisely. N95s can sometimes be used past their expiration date. However, parts like the straps or nose bridge might wear out. This can affect how well the mask fits and seals. So, it's extra important to do a seal check. Masks approved in other countries, like FFP2 and FFP3 masks from the European Union, can also be used. These are similar to NIOSH-approved N95s.
N95 respirators can be reused a few times after being taken off. This is okay as long as they haven't been used in procedures that create a lot of tiny airborne particles. Also, they must not be contaminated with a patient's body fluids. Reusing masks does increase the risk of germs getting on the surface. Manufacturers might suggest a limit on how many times a mask can be used. If there's no guidance, it's suggested to limit reuse to five times to be safe.
When there are very few N95 respirators left, they should be given first to workers doing risky procedures. This includes those working closely with sick patients. In these cases, it's very important for sick patients to wear a surgical mask. Also, keeping a distance from the patient helps reduce the spread of germs. If no respirators are available, workers who are at higher risk of getting very sick might not care for patients. Workers who have already recovered from COVID-19 might be preferred to care for patients. Portable fans with HEPA filters can also help improve air circulation in rooms. If neither respirators nor surgical masks are available, homemade masks might be used as a last resort. However, these masks have not been tested or approved by NIOSH.
The World Health Organization (WHO) suggested ways to reduce the need for masks during the pandemic. These included using telemedicine (doctor visits by video or phone) and using physical barriers like clear windows. They also suggested only allowing essential staff into a patient's room. Using only the necessary protective gear for each task and reusing the same respirator for multiple patients with the same illness were also recommended. They also advised against healthy people wearing masks if they didn't need to.
Scientists have looked into ways to clean N95 respirators during shortages. However, there's a concern that cleaning might make the filter work less well. It could also change the mask's shape, affecting its fit. Researchers at Duke University found a way to clean N95s using vaporized hydrogen peroxide without damaging them. This allows for limited reuse. Battelle also got special permission to sterilize N95 masks. NIOSH suggests that during shortages, N95 respirators can be used up to five times without cleaning. This is true as long as they are not used in procedures that create aerosols. Also, they must not be contaminated with patient body fluids. Wearing a cleanable face shield over an N95 can help reduce contamination. Using clean gloves when putting on a used N95 also helps. Remember to throw away the gloves right after.
N95 Mask vs. Surgical Mask
A surgical mask is a loose-fitting, disposable mask. It creates a physical barrier between the wearer's mouth and nose and possible germs nearby. When worn correctly, a surgical mask helps block large droplets, splashes, or sprays that might contain viruses or bacteria. Surgical masks can also help stop the wearer's saliva and breathing droplets from reaching others.
However, a surgical mask is not designed to filter very small particles in the air. These tiny particles can spread when someone coughs, sneezes, or during certain medical procedures. Surgical masks also don't offer complete protection from germs. This is because they don't fit tightly against the face, allowing gaps. Studies have shown that even surgical masks with good filters might not seal well on many people's faces. This can lead to air leaking in.
The U.S. Centers for Disease Control and Prevention (CDC) recommends surgical masks for procedures where the wearer might create small airborne particles that could harm a patient. The CDC recommends N95 respirators to protect the wearer from breathing in infectious particles. This includes germs like those that cause Mycobacterium tuberculosis, Avian influenza, severe acute respiratory syndrome (SARS), pandemic influenza, and Ebola. Some N95 respirators are also approved by the U.S. Food and Drug Administration as "surgical N95s." These provide breathing protection to the wearer as well.
History of N95 Masks
In the 1970s, the United States Bureau of Mines and NIOSH created standards for single-use respirators. The first N95 respirator was developed by a company called 3M and approved in 1972. 3M used a melt blowing process they had developed years before. This process was used in products like ribbon bows and bra cups. A designer named Sara Little Turnbull helped find many uses for this process. While N95 masks were first made for industrial use, they became more common in healthcare in the 1990s. Many American companies stopped making N95 masks in the 2000s. This was due to legal costs and competition from foreign companies.
During the 2019–20 coronavirus pandemic, N95 masks were in very high demand and short supply. Making N95 masks was difficult because there wasn't enough nonwoven polypropylene fabric. This fabric is the main filter material. Also, China, which makes 50% of the world's masks, stopped exporting them. China needed all its masks for its own fight against the virus. They only allowed exports as government aid.
In March 2020, President Donald Trump used the Defense Production Act against the American company 3M. This law allowed the Federal Emergency Management Agency to get as many N95 respirators as it needed from 3M. White House trade adviser Peter Navarro said there were worries that 3M products were not reaching the U.S. 3M replied that they had not changed their prices. They also said they could not control the prices charged by their dealers or retailers.
In early April 2020, the State of Berlin in Germany claimed that a shipment of 200,000 N95 masks they ordered from 3M's China factory was stopped in Bangkok. Berlin said the masks were sent to the United States instead. Berlin's Mayor Michael Müller blamed President Trump for the masks being taken. The Berlin police president, Barbara Slowik, said she believed it was related to the U.S. government's export ban. 3M denied knowing about the Berlin order. The U.S. government also denied taking any masks. They stated they use proper ways to buy all their supplies.
Images for kids
-
Surgical N95 respirators are approved by NIOSH and cleared by FDA for healthcare use.
See also
 In Spanish: Mascarilla N95 para niños
In Spanish: Mascarilla N95 para niños