Periodontology facts for kids
| Occupation | |
|---|---|
| Specialty | |
|
Activity sectors
|
Dentistry |
| Description | |
|
Education required
|
Dental degree |
|
Fields of
employment |
Hospitals, private practices |
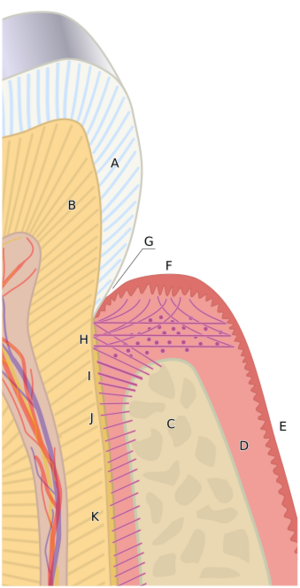
Periodontology or periodontics is a special part of dentistry. It focuses on the structures that support your teeth, like your gums and bones. It also studies diseases and conditions that affect these parts. The supporting tissues are called the periodontium. These include your gums (gingiva), the bone around your teeth (alveolar bone), a layer on the tooth root (cementum), and the periodontal ligament. A periodontist is a dentist who specializes in preventing, finding, and treating periodontal disease. They also place dental implants.
Contents
- What is the Periodontium?
- Common Gum Problems
- Understanding Periodontal Disease
- How Gum Disease Starts (Aetiology)
- How Gum Disease Progresses (Pathogenesis)
- Risk Factors for Gum Disease
- How Gum Disease is Found (Diagnosis)
- How Gum Disease is Treated
- Role of the Oral Health Therapist
- What is a Periodontist?
- Becoming a Periodontist (Training)
- Keeping Your Gums Healthy (Maintenance)
- See also
What is the Periodontium?
The periodontium is a group of structures that surround, support, and protect your teeth. It is mostly made up of gum tissue and the bone that holds your teeth.
Your Gums (Gingiva)
Healthy gums can be light pink or have darker spots. The soft tissues and fibers that cover and protect the tooth root and bone are called the gingivae. They are divided into three types: free, attached, and interdental gingiva. All these parts work to protect your teeth from damage and bacteria.
Free Gingiva: The Gum Edge
The free gingiva is the part of the gum that is above the bone. In a healthy mouth, the gingival margin is the edge of the gum that hugs the tooth. It meets the tooth where the enamel (crown) and cementum (root) join. There is a small, natural space called the gingival sulcus between the tooth and the free gum. In a healthy mouth, this space is usually very shallow (0.5-3mm deep). If you have gum disease, this space can get deeper.
Attached Gingiva: Firm and Strong
The junctional epithelium is like a collar around the tooth at the bottom of the gum space. It separates the free gum from the attached gum. This part creates a special barrier against tiny germs around the gum line. Strong fibers connect the attached gum tightly to the bone and tooth root. This attached gum helps protect your tissues when you chew, brush your teeth, or talk. It is usually pale pink and might have a bumpy texture.
Interdental Gingiva: Between Your Teeth
The interdental gingiva fills the space between two teeth where they touch. It usually looks like a triangle. This part is made of two small gum bumps (papillae). The main job of the interdental gingiva is to stop food from getting stuck between your teeth when you chew.
Alveolar Mucosa: Flexible Tissue
This tissue is located beyond the attached gums. It is not as firmly attached and is redder than the attached gums. It allows your cheeks and lips to move easily.
Periodontal Ligament: Your Tooth's Cushion
The periodontal ligament is a connective tissue. It connects the outer layer of your tooth root (cementum) to the bone around it. It has many strong fibers that act like a cushion. This ligament helps absorb the forces on your teeth when you chew. This protects your teeth inside their sockets.
Alveolar Bone: The Tooth Holder
In a healthy mouth, the alveolar bone surrounds your teeth. It forms the bony socket that supports each tooth. This bone is strong and dense, especially on the outside. Inside, it's a bit spongier.
Cementum: Root Protection
Cementum is the outer layer of your tooth root. It covers the dentine layer and helps the periodontal ligament fibers attach. It also protects the dentine and seals tiny tubes in the tooth. It is not as hard as enamel and is usually light yellow.
Common Gum Problems
Gingivitis is a common condition that affects your gums. It is a type of gum disease, but it's the mildest form. It does not cause lasting damage to your gums, ligaments, or bone. You might notice it if your gums bleed easily when you brush or eat. Your gums might also look swollen, red, and inflamed.
Gingivitis usually doesn't hurt. It's most often caused by plaque (a sticky film of bacteria) building up because of poor oral hygiene. Other things can increase your risk, like uncontrolled diabetes or some medicines. You can reverse gingivitis by brushing and cleaning your teeth better. If left untreated, gingivitis can turn into more serious periodontal disease.
Understanding Periodontal Disease
Periodontal disease includes several conditions that cause the loss of gum attachment and damage to the bone around your teeth.
These diseases often happen when bacteria from plaque build up on your gums and teeth. Your body's immune system also plays a role. If not treated, these diseases can lead to bone loss and even tooth loss. For example, in South Korea in 2013, periodontal disease caused 70.8% of tooth loss in affected patients. In Scotland, it's the second most common reason for losing teeth, after cavities. Brushing twice a day and flossing can help prevent these diseases.
Healthy gums look pale or coral pink in Caucasian people. They might have different colors in other races. The gum edge should be right at the tooth's enamel-cementum line. The space between the tooth and gum should be shallow (1–3mm). Healthy gums also do not bleed when gently checked.
The main cause of periodontal disease is dental plaque. Plaque forms a sticky film of bacteria on your teeth. If you don't remove it well, especially near your gums, your body reacts. This can lead to an imbalance that changes your mouth from healthy to diseased. Other things can also make gum disease worse, like age, how well you clean your teeth, and your diet. Health conditions like uncontrolled diabetes or smoking can also be factors.
Signs and symptoms of periodontal disease include:
- Bleeding gums
- Gums pulling away from teeth (gingival recession)
- Bad breath
- Loose teeth
- Dentures that don't fit well
- Build-up of plaque and hard deposits (calculus)
Things that can increase your risk include:
- Smoking
- Diabetes
- Obesity and low Vitamin D
- Poor oral hygiene
- Heart disease
- Stress
- Genetics (family history)
- Some medications (can cause dry mouth or gum overgrowth)
- Blood disorders
- Pregnancy (can make existing gum problems worse due to hormone changes, but doesn't cause them)
It's important for dental professionals to understand these risk factors. This helps them treat and manage gum diseases effectively.
Types of Periodontal Disease
There are different types of periodontal diseases and conditions. Here are some of them:
- Gingival Diseases: These affect only the gums. They can be caused by plaque or other things.
- Periodontitis: This is a more serious form where the bone and supporting structures are damaged. It can be chronic (slowly progressing) or aggressive (fast progressing).
- Necrotizing Periodontal Diseases: These cause tissue breakdown in the gums.
- Abscesses of the Periodontium: These are infections that form pus in the gum or bone.
- Periodontitis with Other Conditions: Sometimes, gum disease is linked to other health problems or tooth issues.
- Peri-Implant Diseases: These affect the tissues around dental implants.
Preventing Gum Disease
The best way to prevent gum disease is to take care of your teeth at home. This means using the right tooth brushing technique, cleaning between your teeth with floss or interdental brushes, and using fluoride toothpaste. It's also important to visit your dental professional for check-ups and cleanings twice a year.
Treating Gum Disease
Besides specialist treatment, a general dentist or oral health therapist can perform routine cleanings. They use special tools to remove plaque and calculus. They can also teach you how to brush and clean between your teeth better.
How Gum Disease Starts (Aetiology)
The main reason for periodontal disease is plaque biofilm. A biofilm is a community of tiny living things (microorganisms) that stick to a hard surface that doesn't shed, like your teeth.
Here's how plaque forms:
- First, a thin film called a pellicle forms on your teeth.
- Then, bacteria start to stick to this film within an hour or two.
- More bacteria join, sticking to each other and forming a complex community.
- This community grows and matures, especially in hard-to-clean areas.
- These bacteria are protected by a slimy layer, which makes them hard to remove. That's why brushing and cleaning are so important!
The best way to control plaque is to remove it mechanically. This means brushing your teeth, cleaning between them, and having a dental professional clean your teeth.
How Gum Disease Progresses (Pathogenesis)
Your immune system plays a big role in gum disease. Even in a healthy mouth, your body is always fighting off bacteria. White blood cells (like neutrophils) are the main cells that eat bacteria in your gum pockets. They move from your tissues into a special fluid called gingival crevicular fluid (GCF).
When there's too much plaque, these cells can get overwhelmed. They release harmful enzymes that can damage your tissues. This is when your gums become red, swollen, and inflamed, and might bleed when you brush. If this continues, the disease can get worse. More immune cells come, causing more inflammation. This can lead to the breakdown of collagen (a protein in your tissues) and the loss of bone around your teeth. At this point, gingivitis has turned into periodontitis, and the damage to the supporting structures is permanent.
Risk Factors for Gum Disease
A risk factor is something that increases your chance of getting a disease. Some risk factors can be changed (modifiable), and some cannot (non-modifiable).
Modifiable Risk Factors (Things you can change):
- Smoking: Smoking is a major risk factor for gum disease. It harms blood vessels and makes it harder for your gums to heal. It also prevents your immune system from fighting off bad bacteria. Quitting smoking can help prevent gum disease from getting worse.
- Diabetes: If your diabetes is not well-controlled, it can make gum disease worse, and vice versa. Keeping your blood sugar in check is very important for your gum health.
- Obesity and Vitamin D: Being overweight and not getting enough Vitamin D can affect your immune system and bone health, increasing your risk. Eating a healthy diet is important.
- Poor Oral Hygiene: Since plaque is the main cause of gum disease, not brushing and flossing well is the biggest risk factor. Good oral hygiene is key to preventing and controlling gum disease.
- Stress: Long-term stress can weaken your body's defenses against bacteria, making you more likely to develop gum disease.
Non-Modifiable Risk Factors (Things you can't change):
- Genetics: Your genes and how your immune system works can play a role in how likely you are to get gum disease.
- Osteoporosis: This condition makes bones less dense, including the bone around your teeth. More research is needed to fully understand its link to gum disease.
- Medications: Some medicines can have side effects that affect your gums, like causing dry mouth or gum overgrowth. Your dental professional should always review your medical history.
- Pregnancy: Hormonal changes during pregnancy can make existing gum inflammation worse. It's important to keep up good oral hygiene during pregnancy.
Understanding these risk factors helps dental professionals provide the best care.
How Gum Disease is Found (Diagnosis)
To find out if you have gum disease, dental professionals use classification systems. These systems help them categorize gum and periodontal diseases based on how severe they are, what caused them, and how they should be treated.
A diagnosis starts with looking at your medical, dental, and social history. This helps identify any risk factors or other health conditions. Then, the dental professional will examine your mouth. They might use special tools to measure the depth of your gum pockets and check for bleeding. X-rays can also be taken to see the bone levels around your teeth.
How Gum Disease is Treated
Modern gum disease treatment usually follows a four-phase plan. This plan helps ensure that treatment is done in a logical order, which improves your chances of getting better.
Phase 1: Initial Treatment (Getting Control)
This is the first step. The goal is to reduce and get rid of gum inflammation. This is done by removing dental plaque and calculus (hardened plaque). Fixing cavities and broken fillings also helps, as these can trap bacteria. This phase includes cleaning your teeth, teaching you how to brush better, and sometimes temporary fixes for loose teeth.
After 3–6 weeks, your dental professional will check your gums again. They will see how well the first phase worked and if your oral hygiene has improved. They might adjust your treatment plan if needed.
Phase 2: Surgical Treatment
Sometimes, surgery is needed if the gum pockets are very deep, or if there are uneven bone areas. This phase helps manage specific gum pocket situations and can involve procedures to cover exposed roots or remove overgrown gum tissue.
Phase 3: Restorative Treatment
In this phase, any missing teeth or damaged areas are fixed. This might involve crowns, bridges, or other restorations. The goal is to restore your bite and smile.
Phase 4: Maintenance (Keeping Healthy)
This is the most important phase for long-term success. After treatment, you will have regular check-ups and cleanings to prevent the disease from coming back. This phase helps maintain your gum health and involves a long-term relationship with your oral health therapist, dentist, or periodontist.
Standard Treatment Methods
The main treatment for gum disease is non-surgical. This involves a thorough mechanical cleaning to remove calculus and plaque from the tooth surfaces, especially below the gum line. This is called debridement. It helps change the environment in your mouth to a healthier one.
Debridement is usually done with hand tools or ultrasonic devices. It might take a few appointments. After the cleaning, it's crucial for you to keep your teeth clean at home. This means brushing twice a day and cleaning between your teeth daily. Your dental professional will teach you the best ways to do this and help you stay motivated.
Role of the Oral Health Therapist
An oral health therapist is a dental team member who is trained as both a dental hygienist and a dental therapist. They work closely with dentists and specialists like periodontists. They are often involved in treating gum diseases. Their job includes checking your oral health, diagnosing problems, treating them, and helping you maintain your oral health. They also teach you about good oral hygiene. Oral health therapists are important because they specialize in preventing dental problems.
What is a Periodontist?
A periodontist is a specialist dentist who treats patients with gum-related diseases and conditions. They focus on preventing, diagnosing, and treating gum disease. To become a periodontist, they complete extra specialist training after dental school.
Periodontists treat patients with severe gum diseases or complex medical histories. They offer many treatments, including deep cleanings (root scaling and planing), gum surgery, implant surgery, and other complex gum procedures.
Some procedures a periodontist performs:
- Non-surgical treatments
- Gum graft surgery
- Laser treatment
- Procedures to help new tissue grow
- Dental crown lengthening
- Dental implants
- Pocket reduction procedures
- Gum plastic surgery
Your general dentist or oral health therapist will decide if you need to see a periodontist and will give you a referral.
Becoming a Periodontist (Training)
Before you can apply to a periodontology training program, you must first complete a dental degree.
Australia
In Australia, programs are usually three years long. You earn a master's degree (MDS) or a Doctor of Clinical Dentistry (DClinDent).
Canada
Canadian programs are at least three years long and usually lead to a master's degree (MSc or MDent).
Europe
In Europe, the European Federation of Periodontology (EFP) approves post-graduate programs. After three years of full-time training in an approved program, you can get a certificate of specialized training.
India
In India, periodontics is a specialization. You complete a Master of Dental Surgery (M.D.S.) program, which is three years long.
United Kingdom
In the UK, specialist training is either a three-year full-time program or four years part-time. You earn a Master of Clinical Dentistry (MClinDent).
United States
In the U.S., programs approved by the American Dental Association (ADA) are at least three years long. U.S.-trained periodontists specialize in preventing, diagnosing, and treating gum diseases and placing dental implants.
Keeping Your Gums Healthy (Maintenance)
After any gum treatment, whether surgical or non-surgical, ongoing maintenance is essential for long-term health.
Gingivitis Maintenance
Gingivitis is reversible. After removing the plaque or calculus, your gums can heal. You need to thoroughly clean your teeth every day with a soft toothbrush and an interdental aid (like floss or interdental brushes). If you don't keep cleaning, gingivitis can come back and lead to more serious problems.
Necrotizing Ulcerative Gingivitis (NUG) Maintenance
This is a painful type of gum disease where gum tissue breaks down. It causes pain, bleeding, bad breath, and gray-looking gums. Treatment involves cleaning, often with local anesthetic. To maintain health, you might use a special mouthwash (chlorhexidine) and improve your brushing and interdental cleaning. Eating healthy and quitting smoking are also very important. For some patients, antibiotics might be needed.
Chronic Periodontitis Maintenance
This involves inflammation and lasting damage to the bone around your teeth. It usually progresses slowly. Treatment often includes deep cleaning (scaling and root planning) and sometimes surgery. After treatment, regular check-ups and good home care are vital to stop the disease from getting worse. This means brushing twice a day and cleaning between your teeth daily.
Aggressive Periodontitis Maintenance
This type causes fast and severe damage to the gums and bone. It can happen even in people with good oral hygiene and can be genetic. Treatment depends on how severe it is and your age. It might include deep cleaning and antibiotics. Good oral hygiene and regular check-ups every 3–6 months are necessary to prevent it from coming back.
Periodontitis from Systemic Disease Maintenance
Sometimes, gum disease is linked to other health conditions like diabetes or Down syndrome. Treatment depends on the severity and can be surgical or non-surgical. After treatment, it's very important to keep up with your oral hygiene (brushing twice a day, interdental cleaning daily) and manage your systemic health condition.
See also
 In Spanish: Periodoncia para niños
In Spanish: Periodoncia para niños
 | Kyle Baker |
 | Joseph Yoakum |
 | Laura Wheeler Waring |
 | Henry Ossawa Tanner |