Acinetobacter facts for kids
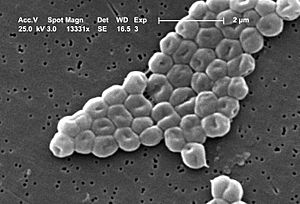
Acinetobacter is a group, or genus, of tiny living things called bacteria. These bacteria are known as Gram-negative and belong to a larger family called Gammaproteobacteria. Acinetobacter bacteria do not react to a certain chemical test (called oxidase-negative). They can move in a special way called twitching motility. When seen under a microscope, they often appear in pairs.
These bacteria are very important in soil. They help break down substances like aromatic compounds, which is a process called mineralization. Some Acinetobacter species, especially Acinetobacter baumannii, can cause infections in people who are already sick or have weak immune systems, particularly in hospitals.
Quick facts for kids Acinetobacter |
|
|---|---|
 |
|
| Acinetobacter baumannii | |
| Scientific classification |
|
| Unrecognized taxon (fix): | Acinetobacter |
| Species | |
|
Acinetobacter albensis |
|
Contents
Understanding Acinetobacter Bacteria
What Acinetobacter Looks Like
Acinetobacter species are aerobic, meaning they need oxygen to live. They do not use fermentation to get energy. They are Gram-negative bacilli, which means they are rod-shaped. When grown on a special dish, they often look like short, oval rods, which is called coccobacillary. In liquid, especially when they are first growing, they tend to be more rod-shaped.
It can be tricky to tell Acinetobacter apart from other bacteria just by looking at them under a microscope. This is especially true when they are taken from human samples.
Most types of Acinetobacter grow well on a special jelly called MacConkey agar. Even though they are usually not considered "lactose-fermenting," they sometimes partly ferment lactose on this agar. They are negative for the oxidase test and indole test. They are positive for the catalase test. They do not move on their own and usually do not reduce nitrate.
Under certain conditions, like when they have lots of carbon but not enough phosphorus or nitrogen, Acinetobacter bacteria can store energy inside themselves. They do this by making special storage molecules called polyhydroxyalkanoates.
Where the Name Acinetobacter Comes From
The name Acinetobacter comes from ancient Greek words. It means "nonmotile rod." The first part, acineto-, means "not moving." The second part, -bacter, refers to a rod-shaped bacterium. So, the name perfectly describes these bacteria as "rods that don't move."
Different Types of Acinetobacter
There are currently 38 officially recognized species within the Acinetobacter group. Each species has its own unique characteristics.
How Scientists Identify Acinetobacter
Identifying specific Acinetobacter species can be difficult. In the past, scientists looked at things like how they grew, their shape, and what they ate. For example, the A. calcoaceticus–A. baumannii group was identified by how they formed smooth, round colonies at a certain temperature. However, these methods could not tell very similar species apart.
Because it's hard to identify every species in a regular lab, Acinetobacter are often grouped into three main categories:
- Acinetobacter calcoaceticus-baumannii complex: These bacteria use glucose and do not cause hemolysis (breaking down red blood cells).
- Acinetobacter lwoffii: These bacteria do not use glucose and do not cause hemolysis.
- Acinetobacter haemolyticus: These bacteria cause hemolysis.
Scientists can also use a special test called a chromosomal DNA transformation assay. This test checks if the bacteria can take up DNA from another Acinetobacter species. If they can, it confirms they belong to the Acinetobacter group.
More advanced methods use molecular biology techniques. These methods look at the bacteria's DNA to find unique patterns. Techniques like pulsed field gel electrophoresis (PFGE) and multilocus sequence typing (MLST) are used to identify species and understand how different strains are related.
Where Acinetobacter Lives
Acinetobacter bacteria are found almost everywhere in nature. They commonly live in soil and water. They are very tough and can survive on both wet and dry surfaces. They can also survive after being exposed to many common cleaning products. This toughness allows some Acinetobacter species to live in places like hospitals. They can also grow in a wide range of temperatures, which helps them survive in many different environments.
Acinetobacter and Our Health
Acinetobacter bacteria are often found in hospital-acquired infections. These are infections that people get while they are being treated in a hospital. They are especially common in intensive care units (ICUs). Both single cases and larger outbreaks can happen.
Common Infections Caused by Acinetobacter
A. baumannii is a common cause of hospital-acquired pneumonia, which is a lung infection. This is especially true for pneumonia that develops later during a hospital stay or is linked to breathing machines. These bacteria can also cause other infections. These include skin and wound infections, bacteremia (bacteria in the bloodstream), and meningitis (an infection of the brain and spinal cord lining). However, A. lwoffii is more often linked to meningitis.
A. baumannii is the main Acinetobacter species that causes human illness. It has been linked to many hospital-acquired infections. These include bloodstream infections, urinary tract infections (UTIs), and infections of wounds and burns. Patients in ICUs often get pneumonia caused by A. baumannii. Risk factors include being on a breathing tube for a long time. The bacteria can sometimes enter the bloodstream, leading to serious complications. UTIs caused by A. baumannii are often linked to the use of catheters and antibiotic treatments. A. baumannii can also infect skin and soft tissues after injuries or surgeries. It commonly infects burns, making treatment difficult. In rare cases, it can cause meningitis, especially after surgery, or serious infections in newborns.
Why Acinetobacter Can Be Hard to Treat
A big challenge with A. baumannii is that it can become resistant to many antibiotics. This means the medicines that usually kill bacteria no longer work. It has developed resistance to common antibiotics like cephalosporins, β-lactam antibiotics, aminoglycosides, and quinolones. Resistance to carbapenems, which are strong antibiotics, is also becoming more common.
A. baumannii can survive on human skin or dry surfaces for weeks. It is also resistant to many disinfectants. This makes it very easy for the bacteria to spread in hospitals. This puts people with weakened immune systems at risk for infections that are hard and costly to treat. Bacteria can also share their antibiotic resistance genes with other harmful bacteria. This happens through a process called horizontal gene transfer.
Interestingly, in healthy people, Acinetobacter on the skin might be linked to fewer allergies. Some scientists think it might help protect against allergies.
Preventing Acinetobacter Infections
Good hygiene practices are very important in hospitals. This includes thorough handwashing and cleaning surfaces. These steps help prevent the spread of Acinetobacter and other germs. Some hospitals have even used special air purifiers to reduce airborne Acinetobacter infections.
Treating Acinetobacter Infections
Acinetobacter species are naturally resistant to many types of antibiotics. These include penicillin, chloramphenicol, and often aminoglycosides. They can also develop resistance to fluoroquinolones during treatment. This resistance can spread to other types of drugs.
The Centers for Disease Control and Prevention (CDC) has reported a big increase in antibiotic resistance in Acinetobacter strains. Carbapenems are often considered a last resort treatment. Acinetobacter species are unusual because they are sensitive to sulbactam. Sulbactam is often used to help other antibiotics work better, but it also has its own antibacterial properties against Acinetobacter.
New Ways to Fight Acinetobacter
Recently, a new antibiotic combination called sulbactam-durlobactam (marketed as Xacduro) was approved for medical use in the United States in May 2023. This new medicine has shown good results against A. baumannii strains that are resistant to carbapenems.
Infections with multidrug-resistant A. baumannii have been a concern in hospital settings, including those treating injured service members. For very resistant infections, an older antibiotic called colistin (polymyxin E) has sometimes been used.
Scientists are also exploring other ways to fight these bacteria. One idea is phage therapy, which uses viruses that specifically infect and kill bacteria. Another approach involves using special molecules called gene-silencing antisense oligomers. These molecules can stop the bacteria from growing.
Bacteria can share DNA with each other in a process called natural transformation. This means one bacterium can take up DNA from its surroundings. This DNA might come from another bacterium that has died. For Acinetobacter calcoaceticus, this ability to take up DNA is triggered when a growing culture is diluted into fresh food.
This DNA transfer can help bacteria repair damage to their own DNA. It is also a way for them to exchange genetic information. This sharing of DNA can help Acinetobacter adapt and survive in different environments.
 | William M. Jackson |
 | Juan E. Gilbert |
 | Neil deGrasse Tyson |

