Asthma facts for kids
Asthma is a common health problem that affects the airways in your lungs. It makes the inside of your airways swell up. Asthma also causes the muscles around your airways to get tight and narrow. This makes it hard for enough air to pass through, so you can't breathe normally.
During an asthma attack, special cells in your airways make too much sticky mucus. This extra mucus blocks the airways even more, making it super hard to breathe.
If someone is having an asthma attack, they often make a wheezing sound when they try to breathe. This is the sound of air squeezing through those narrow airways. They might also feel short of breath, meaning they can't take a full, deep breath. Their chest might feel tight, like it's being squeezed. They may also cough a lot.
Asthma attacks can be serious and need quick medical help. In some cases, they can even be fatal (cause someone to die). There's no cure for asthma, but there are treatments like medicines to help people manage it. There are also things people with asthma can do to keep their asthma from getting worse.
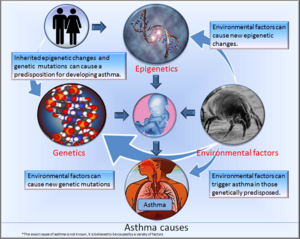
Many things can increase your chances of getting asthma. Scientists are still learning the exact reasons. Some factors are believed to be passed down through your genes from your parents. This means you might inherit certain changes in your genes that make you more likely to develop asthma. Epigenetics are changes in how your genes work, even if the genes themselves don't change. These changes can also be inherited or happen when a baby is growing inside its mother, or during childhood.
Contents
What Causes Asthma?
The exact cause of asthma isn't fully known. It's thought to be a mix of different reasons:
Your Genes and Asthma
When there are changes in a person's genes (called mutations), these changes can be passed down to their children. If one or both parents have these gene changes, their children might be born with them. These changes can make a person more likely to get certain diseases, like asthma. For some diseases, one gene change might be enough. But for asthma, it's often changes in many different genes that increase the chance.
How Genes Work (Epigenetics)
Epigenetic changes affect how your genes "express themselves" or work, but they don't actually change the DNA of the gene itself. These changes can be inherited, or they can happen when a baby is still inside its mother. They can also happen during childhood because of things like a lung infection, being around certain chemicals or drugs, or even your diet. These changes can be passed down for a generation or two, but they aren't permanent. Even though they affect how your genes work, they don't permanently change your genes. Scientists believe epigenetic changes can also make someone more likely to get asthma.
Things Around You (Environmental Factors)
Environmental factors are things in your surroundings that can affect your health. Unhealthy environmental factors include living where there's a lot of air pollution, having many bugs in your house, or being around cigarette smoke.
If someone has gene changes that make them more likely to get asthma (a genetic predisposition), and they also live in unhealthy surroundings, like a home with lots of dust mites, they are even more likely to develop asthma.
Atopy and Allergies
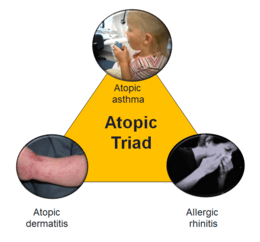
Atopy happens when there are changes in some of the genes you're born with. These gene changes make your body produce more of a special type of antibody called Immunoglobulin E (IgE). People with atopy are also more sensitive to things like chemicals, smoke, and dust (called environmental antigens). This hypersensitivity means they are more allergic to things in the environment than people who don't have these gene changes.
This hypersensitivity makes their body react in certain ways. People who are atopic often develop allergic rhinitis, which affects the passages behind the nose. They are also more likely to get atopic dermatitis (skin rashes) and atopic asthma. Up to 40% of people with allergic rhinitis also have asthma. These three problems – allergic rhinitis, atopic dermatitis, and atopic asthma – are sometimes called the Atopic Triad (a triad means a group of three). People who are atopic might also have other problems like food allergies, insect sting allergies, hives (urticaria), and other skin rashes.
If one of your parents is atopic, you have a good chance of being atopic too. If both parents are atopic, your chances are even higher.
Acetaminophen and Asthma
Some studies have found a possible link between acetaminophen (like Tylenol) and asthma. For example, a large study in 2008 showed that children who took acetaminophen for a fever during their first year of life had a 50% higher chance of getting asthma later on. The more acetaminophen children took, the higher their risk. Some doctors suggest that children with asthma, or those at risk, should try to avoid acetaminophen.
Types of Asthma
Atopic Asthma
Atopic asthma is the most common type of asthma. It's linked to allergies, as explained above.
Cough-Variant Asthma
In cough-variant asthma, a cough is the main, and sometimes only, sign. This type of asthma usually doesn't cause wheezing or shortness of breath. It often causes a dry, scratchy cough with little or no phlegm. About 30% of people with cough-variant asthma will later develop typical asthma.
Work-Related Asthma
Work-related asthma is caused or made worse by irritants in a person's workplace. Jobs that might cause this type of asthma often involve a lot of smoke or chemicals. There are different kinds of work-related asthma:
- Occupational asthma with latency: This happens when asthma symptoms appear after some time (latency) after being exposed to irritants at work. For example, if someone starts a factory job in January and develops asthma symptoms in March, the time between January and March is the latency period.
- Irritant-Induced Asthma (IIA): Here, asthma symptoms can start right away (without latency) after being exposed to irritants. For example, if a janitor starts using ammonia and immediately finds it hard to breathe, that's IIA.
- Work-aggravated asthma: This is when someone already has asthma, and things at their job make it worse.
Exercise-Induced Asthma
Exercise-induced asthma (EIA) is also called exercise-induced bronchospasm. This is when exercise is the main, or only, trigger for an asthma attack. If someone already has another type of asthma or is atopic, they are more likely to get EIA.
Nocturnal Asthma
Nocturnal means "at night." Nocturnal asthma is when asthma symptoms get worse during the night.
Premenstrual Asthma (PMA)
Premenstrual asthma (PMA) is when asthma symptoms get worse during the time before a menstrual period. This can affect up to 40% of females with asthma. To diagnose PMA, doctors look at a detailed history of menstrual cycles and asthma symptoms. Keeping a diary of symptoms can be very helpful.
Status Asthmaticus
Status asthmaticus is a very severe form of asthma. In this case, an asthma attack keeps getting worse, and the usual asthma medicines don't work. Status asthmaticus can be fatal and is a medical emergency.
Signs and Symptoms of Asthma
In medicine, signs and symptoms are how a health problem affects a person's body. Sometimes, asthma signs and symptoms are mild and don't bother the person much. Other times, they can be severe and make the person feel very sick.
Not everyone with asthma has all the signs and symptoms all the time. Someone might have certain symptoms during one attack and different ones during another. Some people with asthma might go a long time between attacks with no symptoms, while others might have some symptoms every day that get worse during an attack. It also depends on the type of asthma and how mild, moderate, or severe it is.
Some people only have symptoms at certain times, like those with exercise-induced asthma, where exercise triggers the symptoms. For others, asthma symptoms might be triggered or made worse (exacerbated) when they have a cold or other viral infections.
Early warning signs of an asthma attack are physical changes you might notice before an attack fully starts. Knowing these signs can help you take steps to prevent an attack or keep it from getting worse.
Early Warning Signs
Early warning signs of asthma can include:
- Coughing a lot, especially at night.
- Getting out of breath easily.
- Shortness of breath: This means you can't take a deep breath and fill your lungs all the way. You might only be able to take short, shallow breaths. When you're short of breath, your chest might also feel tight.
- Getting tired easily during exercise and feeling weak, wheezing, or coughing after exercise.
- Feeling like a cold or allergies are starting, with sneezing, a runny or stuffy nose, coughing, sore throat, or headache.
Asthma Triggers
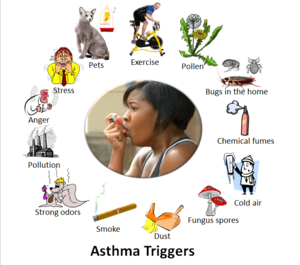
A trigger factor or trigger is something that causes the signs and symptoms of a medical condition to start in someone who already has that condition. Common asthma triggers include:
- Tobacco smoke: You don't have to smoke yourself. Second-hand smoke (smoke from someone else's cigarette, cigar, or pipe, or the smoke they breathe out) can trigger an asthma attack.
- Pets: Animals give off tiny particles called allergens (a type of protein) that people can be allergic to. These allergens can irritate your airways and trigger an asthma attack. Allergens are found in pet dander (dead skin flakes), urine, feces, saliva, and sebum (oily stuff from skin glands). When these dry, their proteins can float in the air and be breathed in. Common pets that can trigger asthma include dogs, cats, hamsters, and birds.
- Bugs: Different types of bugs found in homes can trigger asthma attacks. Like pets, they give off proteins that become airborne allergens. Common bugs that trigger asthma include dust mites, cockroaches, bedbugs, and fleas.
- Fungus spores (mold): Fungi reproduce by releasing spores into the air. If you breathe in these spores, they can trigger asthma. A common type of fungus found indoors and outdoors is aspergillus.
- Strong emotions: Feelings like anger, stress, and even laughter can make asthma symptoms worse.
- Outdoor air pollution: This can come from many sources, like car and truck fumes in busy areas, or chemicals in the air near factories.
- Weather changes: Sudden changes in air temperature can trigger an attack, not just cold air. For example, going from cold outside air into a warm house can cause a bronchospasm (tightening of airways). Sudden changes in humidity also play a part.
The best way to deal with asthma triggers is to learn what they are and avoid them if you can. If you can't avoid them completely, you can adjust your actions. For example, running in cold weather right up to a warm house and going straight inside might cause an attack. Being aware of your environment, both indoors and outdoors, is important when you have asthma.
What Happens During an Asthma Attack?
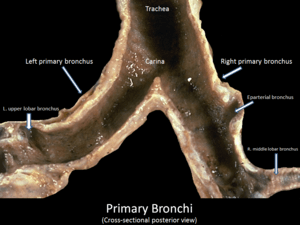
An asthma attack is when your asthma suddenly gets worse, usually after you've been exposed to one or more triggers. When an attack happens, the tissue inside your airways swells up because of inflammation. This is your body's way of trying to protect itself from harmful things like germs or irritants. When the tissues swell, the opening (called the lumen) in your airway gets very narrow.
The smooth muscles (muscles you don't control, like those in your arm) around your airways (bronchi and bronchioles) start to spasm or tighten. This makes the airway opening even narrower. This tightening is called a bronchospasm.
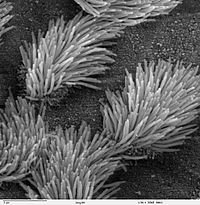
Inside the lining of your airways are glands and cells that make mucus. In healthy lungs, mucus is a thin film that traps irritants like dust or pollen, stopping them from reaching your air sacs.
Your airways also have tiny hairs called cilia. These cilia wave back and forth like little whips, helping to push the mucus and trapped particles up your airways so you can cough them out.
During an asthma attack, the mucus-making glands and cells produce much more mucus than normal, and it's also thicker. This makes it very hard for the cilia to do their job and clear the mucus. So, you have too much mucus, and it's not being moved out. Since your airways are already narrow from swelling and muscle tightening, the extra mucus blocks them even more. This makes breathing very difficult. In very severe attacks, the airways can become completely blocked, making it impossible to breathe.
It's important to learn other signs of breathing difficulty, especially for babies and young children who can't tell you they're having trouble.

Some other signs of an asthma attack include:
- Chest and neck retractions: This happens when muscles in your chest and neck that you don't normally use much for breathing start to pull in. Your body is trying hard to get more air because it's difficult to breathe normally. This causes the skin between your ribs, in your neck, or around your breastbone to sink in when you breathe.
- Nasal flaring: This is when your nostrils get wider than normal when you breathe. It's often a sign that you're having trouble breathing.
- Blue lips and fingertips: Oxygen in the air we breathe makes blood red. Blood without oxygen looks blue. During an asthma attack, it's hard for your body to get enough oxygen. As less oxygen reaches your blood, you have less red blood and more blue blood. The blue color in your lips and under your fingernails is because of this blue blood showing through tiny blood vessels. When parts of your body turn blue from lack of oxygen, it's called cyanosis.
- Sweating: You might notice sweating, especially on your forehead. Your skin might feel cool and clammy (damp and sticky) to the touch.
- Rapid breathing (tachypnea): Breathing in and out much faster than normal.
- Rapid heart beat (tachycardia): Your heart starts beating much faster than normal.
How Doctors Diagnose Asthma
Doctors diagnose asthma based on:
- Your medical history: This includes information about the asthma signs and symptoms you've had.
- Your family medical history: Has anyone in your family had asthma or related conditions, like allergies?
- A physical exam and tests: The doctor will examine you and might order some tests.
Diagnostic Tests
There isn't one single test that can tell for sure if someone has asthma. However, some tests can help with the diagnosis when combined with your medical history and physical exam.
- Lung function tests (Pulmonary function tests or PFTs):
- Spirometry: This test measures how much air your lungs can breathe in and out, and how fast you can breathe out.
- Bronchoprovocation test: In this test, doctors try to make your airways (bronchi and bronchioles) tighten up (have a bronchospasm) to see how sensitive they are. They might ask you to exercise, breathe cold air, or breathe in a special chemical called methacholine. The results are checked using spirometry.
Other Conditions with Similar Symptoms
Differential diagnoses are other medical problems that can cause similar symptoms. Before a doctor makes a final diagnosis, they consider what other conditions might be causing the problem and make sure it's not one of them.
Conditions that can have symptoms similar to asthma include:
- Bronchiectasis (a lung condition)
- Chronic obstructive pulmonary disease (COPD)
Airway Remodeling
Airway remodeling means there are permanent physical changes to the airways that also affect how they work. This can happen after having asthma for a long time. After repeated cycles of inflammation, damage, and repair in the airways, their physical structure can change permanently. This leads to:
- Permanent airway narrowing: The airways are always narrower than normal, and they get even narrower during an asthma attack.
- Easily triggered bronchospasms: The airways become very sensitive and tighten up more easily.
- Fluid in the airway (airway edema).
- Too much mucus (mucus hypersecretion).
- Build-up of collagen: This is a type of protein that can make the airways stiffer.
Airway remodeling has been seen in children as young as six years old.
Not managing asthma properly can lead to airway remodeling. This can increase the risk of dying from an asthma attack. One big problem that leads to poor asthma management is not using the asthma inhaler correctly. Often, this happens because the person with asthma hasn't received proper instructions on how to use it.
More Mucus-Making Cells
One of the physical changes in airway remodeling is having more mucus-making cells than normal. These cells make mucus that protects the airways by trapping harmful particles. Normally, mucus is a thin film. Tiny hairs called cilia move the mucus and trapped particles up the airways.
During an asthma attack, these cells make too much mucus, and it's thicker than normal, making it hard for the cilia to clear it. When airway remodeling happens, your body might make many more mucus-making cells, meaning even more mucus is produced. There might be too much mucus for the cilia to clear, and the airway can become blocked. This is one reason why people with airway remodeling often have more severe asthma. In very serious cases, the airway can become completely blocked, leading to asphyxia (not being able to breathe at all).
Asthma Treatment
A woman using a metered-dose asthma inhaler (or just inhaler for short), which has medicine to treat an asthma attack inside. When the inhaler is put in the mouth and pressed, the medicine is sprayed into the throat and then enters the lungs.
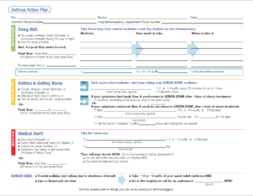
An asthma action plan or management plan, is used to help a person with their asthma. It shows what kind of medicines to take, and when to take them. How to take care of their asthma everyday, AND how to take care of their asthma when it gets worse, or when they have an asthma attack. It helps them know when it is time to call the doctor or go to the emergency room.
Asthma can usually be controlled by avoiding triggers and using certain drugs. Most people with asthma carry special medicines called inhalers with them. The medicine inside the inhaler helps open the tubes that go to the lungs. Inhalers are used to prevent an asthma attack or to stop one that's already happening.
- Rescue medicine: This is an inhaler (sometimes called a "puffer") that you use if you think you're having an asthma attack. It works quickly to open your airways.
- Controller medicine: This is a medicine, either a pill or an inhaler, that you take every day to help prevent asthma attacks from happening.
Hospital Treatment for Severe Attacks
In an emergency, when regular treatments don't work, hospitals have other options:
- Oxygen
- Stronger medicines that work like an asthma spray
- Medicines given through an IV (into a vein)
- Steroids
- Breathing aids (like tubes in very severe cases)
Medicines That Can Make Asthma Worse
Some medicines can make asthma worse or even trigger an attack. These should only be used in very specific situations. Some examples are:
- Non-steroidal anti-inflammatory drugs (NSAIDs): Aspirin is an NSAID. Some people are allergic to it or might have a higher risk of becoming allergic, even if they've used it before.
- Beta blockers: These are medicines used to treat heart problems, but people with asthma should usually not take them.
- Acetaminophen: This pain reliever is believed by some to not only cause asthma but also make it worse in people who already have it. Acetaminophen is often added to other medicines, so always read labels.
- ACE Inhibitors: These medicines are usually for high blood pressure and heart disease. They usually don't make asthma worse, but rarely, they can cause asthma-like symptoms (like coughing) in the first few weeks.
- Sleeping pills and tranquilizers: People with asthma should generally avoid these.
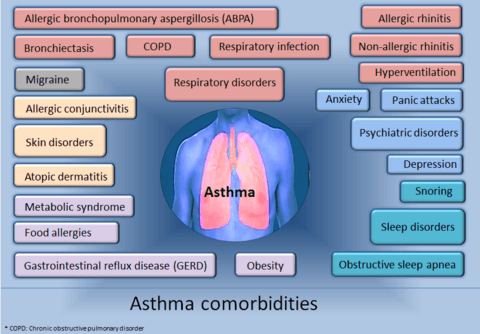
Other Health Problems with Asthma
Often, having one medical problem makes it more likely you'll also have one or more other health issues. These other problems are called "comorbidities." Many different medical and mental health conditions can occur with asthma.
Breathing Problems
- Chronic obstructive pulmonary disorder (COPD)
- Respiratory infections (like colds or flu)
- Chronic sinusitis (long-term sinus infections)
- Rhinitis (allergic or non-allergic runny nose)
- Hyperventilation syndrome (breathing too fast or too deeply)
- Allergic bronchopulmonary aspergillosis (ABPA): A lung disorder caused by an allergic reaction to a fungus called Aspergillus fumigatus.
Stomach and Digestion Problems
- Gastroesophageal reflux disease (GERD), also known as acid reflux or heartburn.
- Eosinophilic esophagitis (EE), a problem where certain cells build up in the food pipe.
Mental Health Problems
- Depression
- Anxiety disorders, including panic disorder.
Sleep Problems
- Obstructive sleep apnea (when breathing stops and starts during sleep).
Skin Problems
- Atopic dermatitis (AD), a type of eczema.
Asthma Around the World
In medicine, epidemiology is the study of what causes diseases, how often they happen, where they happen, and who gets them.
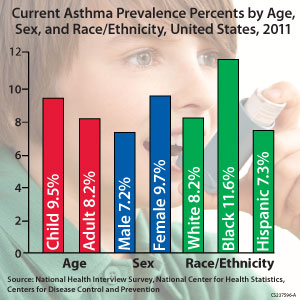
Asthma is more common in richer countries than in developing countries. The United States and Canada have some of the highest asthma rates in the world, even though they are wealthy countries. In Africa, South Africa has the highest asthma rate on the whole continent, even though it's one of the richest countries there.
More than 80% of people who die from asthma are usually from low and middle-income countries. However, South Africa has the fourth highest death rate from asthma in the world, despite being a richer country. In the United States, death rates from asthma are higher for females, adults, and people of African descent.
As of 2011, between 235 and 300 million people worldwide were affected by asthma. About 250,000 people die from the disease each year. The rates vary between countries, with 1% to 18% of the population affected.
The number of asthma cases reported each year increased a lot between the 1960s and 2008. In richer countries, asthma rates have stayed about the same since the mid-1990s, but they have recently increased in developing countries. Asthma affects about 7% of people in the United States and 5% in the United Kingdom. Canada, Australia, and New Zealand have higher rates, around 14–15%.
Images for kids
-
Salbutamol metered dose inhaler commonly used to treat asthma attacks.
-
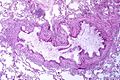
Obstruction of the lumen of a bronchiole by mucoid exudate, goblet cell metaplasia, and epithelial basement membrane thickening in a person with asthma.
See also
 In Spanish: Asma para niños
In Spanish: Asma para niños
 | Kyle Baker |
 | Joseph Yoakum |
 | Laura Wheeler Waring |
 | Henry Ossawa Tanner |