Alexander Fleming facts for kids
Quick facts for kids
Sir Alexander Fleming
FRS FRSE FRCS
|
|
|---|---|

Sir Alexander Fleming in his laboratory at St Mary's, Paddington, London (1943).
|
|
| Born | 6 August 1881 Darvel, East Ayrshire, Scotland
|
| Died | 11 March 1955 (aged 73) London, England
|
| Resting place | St. Paul's Cathedral |
| Citizenship | British |
| Alma mater |
|
| Known for | Discovery of penicillin and Lysozyme |
| Awards |
|
| Scientific career | |
| Fields | Bacteriology, immunology |
| Signature | |
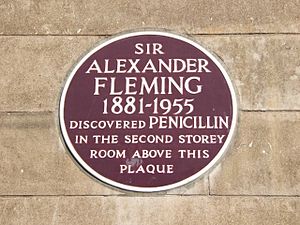
Sir Alexander Fleming (born August 6, 1881 – died March 11, 1955) was a Scottish biologist and pharmacologist. He is famous for discovering penicillin in 1928. Penicillin is a type of antibiotic, which are medicines that fight infections caused by bacteria.
Fleming shared the Nobel Prize in Physiology or Medicine in 1945 for this important discovery. He shared it with Howard Walter Florey and Ernst Boris Chain. His accidental finding of penicillin changed medicine forever. It led to the development of all the antibiotics we use today.
During World War I, Fleming was a captain in the Royal Army Medical Corps. He saw many soldiers die from infections after being wounded. This experience made him want to research bacteriology (the study of bacteria) after the war. He later studied how to use penicillin to help people.
Fleming passed away from a heart attack in London. He was buried in St. Paul's Cathedral.
Alexander Fleming: Discoverer of Penicillin
Early Life and Education
Alexander Fleming was born on August 6, 1881. He grew up on Lochfield farm near Darvel, Scotland. He was one of four children from his father's second marriage. His father, Hugh Fleming, died when Alexander was only seven years old.
Fleming went to local schools in Scotland. He later moved to London to attend the Royal Polytechnic Institution. After working for four years, he inherited some money from his uncle. His older brother, Tom, was a doctor and suggested Alexander become one too.
So, in 1903, Fleming started studying at St Mary's Hospital Medical School in Paddington. He graduated with honors in 1906.
Becoming a Bacteriologist
Fleming was part of the rifle club at his medical school. The club's captain wanted him to stay on the team. So, he suggested Fleming join the research department at St Mary's. There, he became an assistant to Sir Almroth Wright. Wright was a leader in studying vaccines and how the body fights disease.
In 1908, Fleming earned a degree in Bacteriology. He then became a teacher at St Mary's until 1914.
During World War I, Fleming served as a lieutenant and then a captain in the Royal Army Medical Corps. He worked in hospitals on the battlefield in France. In 1918, he returned to St Mary's Hospital. He became a Professor of Bacteriology at the University of London in 1928.
How Antiseptics Worked
During World War I, Fleming saw many soldiers die from infected wounds. Doctors used Antiseptics to treat these wounds. But Fleming noticed that antiseptics often made the injuries worse.
In 1917, he wrote an article explaining why. Antiseptics worked on the surface of wounds. But deep wounds often had bacteria hidden inside. The antiseptics couldn't reach these bacteria. Also, antiseptics sometimes killed helpful things in the body that fought infection. Even with Fleming's findings, many army doctors kept using antiseptics.
Discovery of Lysozyme
Fleming continued his research on bacteria at St Mary's Hospital. He was known for being a bit untidy in his lab. This untidiness actually helped him make important discoveries!
In late 1921, he was working with agar plates (dishes used to grow bacteria). He found that one plate was accidentally contaminated with bacteria from the air. When he added some of his own nasal mucus to the plate, he saw something amazing. The mucus stopped the bacteria from growing around it.
He then tested tears from his co-workers. He found that tears also killed bacteria very quickly. He called this antibacterial substance "Lysozyme." He found lysozyme in many body fluids, like tears, saliva, and egg whites.
Fleming presented his discovery in 1922. But most people didn't think it was very important. This was because lysozyme only worked against harmless bacteria. It didn't affect the dangerous ones that caused serious diseases. However, we now know that lysozyme is a key part of our body's natural defense system.
Discovery of Penicillin
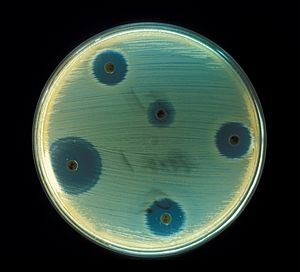
Fleming was studying a type of bacteria called Staphylococcus aureus in 1928. He went on holiday and left some of his culture plates on a bench. When he came back on September 3, 1928, he noticed something strange.
One of his plates was contaminated with a mold. But around the mold, the staphylococci bacteria had been destroyed! He famously said, "That's funny." He realized the mold was killing the bacteria.
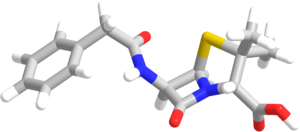
Fleming identified the mold as being from the Penicillium family. He grew the mold in a pure culture. He found that the liquid from the mold contained a powerful antibacterial substance. He tested it on many types of bacteria. It worked against bacteria that cause diseases like scarlet fever, pneumonia, and meningitis.
After calling it "mould juice" for a while, he named it "penicillin" on March 7, 1929. The laboratory where he made this discovery is now the Alexander Fleming Laboratory Museum.
Early Challenges and Doubts
Fleming presented his discovery in 1929. But it didn't get much attention. The main problem was that it was very hard to produce penicillin in large amounts. It was also difficult to get the pure antibacterial compound from the mold. Because of these challenges, penicillin was largely forgotten for many years.
Even in 1936, when Fleming spoke about penicillin's medical importance at a big meeting, no one believed him. People didn't see its potential to treat human infections. Fleming was disappointed but kept working on penicillin.
Purification and Mass Production
Years later, in Oxford, Ernst Boris Chain and Edward Abraham began studying penicillin's structure. They figured out how to purify it. Norman Heatley found a way to make enough of the drug for animal testing.
Many people at the Sir William Dunn School of Pathology in Oxford worked together to produce penicillin. By 1940, they had a stable form of penicillin. They started testing it on people, and it worked amazingly well! This led to efforts to produce penicillin in large quantities.
Fleming was humble about his role. He praised Florey and Chain for turning his lab discovery into a useful medicine. But Fleming was the first to find its properties and give it its name. He also kept the original mold alive for 12 years.
The discovery of penicillin and its development into a widely used medicine marked the beginning of modern antibiotics.
Medical Use and Impact
Fleming tried to treat a patient with a severe sinus infection in 1929. But it didn't work because the infection was caused by a type of bacteria that penicillin couldn't kill.
The first successful medical use of penicillin was by Cecil George Paine, one of Fleming's former students. In 1930, Paine used penicillin to cure eye infections in an adult and three babies. Fleming himself successfully treated a severe eye infection in 1932.
Despite some claims, Fleming continued his penicillin research throughout the 1930s. He tried to find better ways to produce it.
In 1942, Fleming used a purified penicillin sample from Florey to treat a patient named Harry Lambert. Lambert had a life-threatening infection of the nervous system. Fleming gave him the penicillin directly into his spinal canal. Lambert quickly recovered. This was a huge medical breakthrough!
Because of this success, the British government started a committee to mass-produce penicillin. By D-Day in 1944, enough penicillin was made to treat all the wounded Allied soldiers.
Antibiotic Resistance
Fleming quickly noticed a problem: bacteria could become resistant to penicillin. This happened if too little penicillin was used or if it was used for too short a time.
He warned people about this in his speeches. In 1945, he said that if people were careless with penicillin, they could cause bacteria to become resistant. This could lead to deaths from infections that penicillin used to cure. He advised people to only use penicillin when truly needed, and always to use enough for the right amount of time.
He predicted that if penicillin became easily available, people might not use it correctly. This could make microbes resistant. This warning is still very important today as antibiotic resistance is a major global health concern.
Personal Life
On December 24, 1915, Fleming married Sarah Marion McElroy, a nurse from Ireland. They had one son, Robert, who became a doctor. After Sarah passed away in 1949, Fleming married Amalia Koutsouri-Vourekas, a Greek colleague, in 1953.
Fleming was upset when he learned that the method for producing penicillin was patented in the US in 1944. He believed penicillin should be free for everyone's benefit, not a way for companies to make money.
Death
Sir Alexander Fleming died on March 11, 1955, from a heart attack in London. His ashes are buried in St Paul's Cathedral.
Images for kids
-
Sir Alexander Fleming (center) receiving the Nobel Prize from King Gustaf V of Sweden (right) in 1945.
-
A postage stamp from the Faroe Islands honoring Fleming.
See also
 In Spanish: Alexander Fleming para niños
In Spanish: Alexander Fleming para niños
 | Precious Adams |
 | Lauren Anderson |
 | Janet Collins |