Artemisinin facts for kids
 |
|
 |
|
|
Artemisinin
|
|
| Systematic (IUPAC) name | |
| (3R,5aS,6R,8aS,9R,12S,12aR)-Octahydro-3,6,9-trimethyl-3,12-epoxy-12H-pyrano[4,3-j]-1,2-benzodioxepin-10(3H)-one | |
Quick facts for kids Identifiers |
|
| CAS number | 63968-64-9 |
| ATC code | P01BE01 |
| PubChem | 68827 |
| ChemSpider | 62060 |
| Chemical data | |
| Formula | C15H22O5 |
| Mol. mass | ? |
| SMILES | eMolecules & PubChem |
| Synonyms | Artemisinine, qinghaosu |
| Physical data | |
| Density | 1.24 ± 0.1 g/cm³ |
| Melt. point | 152–157 °C (306–315 °F) |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | Oral |
Artemisinin is a powerful medicine used to treat malaria. Malaria is a serious disease caused by tiny parasites called Plasmodium falciparum. Artemisinin and its related medicines are now the main treatment for malaria around the world.
This important drug was found in 1972 by a scientist named Tu Youyou. She later won the 2015 Nobel Prize in Physiology or Medicine for her amazing discovery. Artemisinin comes from a plant called Artemisia annua, also known as sweet wormwood. This plant has been used in Traditional Chinese medicine for a long time. Scientists can also make a part of artemisinin using special engineered yeast. This method is much more efficient than growing the plant.
Artemisinin medicines have a special part called a peroxide bridge. This unique part helps them fight malaria parasites. These drugs are good because they work very fast. They can kill all stages of the malaria parasite's life cycle. However, they can be expensive. Also, the body uses them up quickly. Because of this, artemisinin is usually given with other anti-malaria drugs. This combination helps prevent the parasites from becoming resistant to the medicine. The World Health Organization (WHO) strongly recommends using artemisinin with other drugs, not by itself.
Contents
How Artemisinin Fights Malaria
The World Health Organization (WHO) suggests using artemisinin or its related medicines as the first choice for treating all types of malaria. Usually, it's given along with another drug that lasts longer in the body.
Treating Simple Malaria Cases
For malaria that is not severe, the WHO recommends taking artemisinin-based combination therapies (ACTs) by mouth for three days. These combinations include drugs like artemether/lumefantrine or artesunate/amodiaquine. The artemisinin part quickly kills the parasites. The other drug then finishes off any remaining parasites. It also helps protect against getting infected again.
Treating Severe Malaria Cases
If someone has severe malaria, the WHO suggests giving them artesunate through a vein (intravenous) or into a muscle (intramuscular). This treatment lasts for at least 24 hours. Once the person feels better, they switch to taking the ACT pills for three days. If artesunate is not available, a similar drug called artemether can be given by injection. For young children (under six) with severe malaria, if injections aren't possible, artesunate can be given rectally. After this, they should be taken to a hospital for more care.
Artemisinin is not used to prevent malaria. This is because it leaves the body very quickly. To prevent malaria, you would need to take it many times a day.
When Not to Use Artemisinin
The WHO advises pregnant women in their first three months of pregnancy to avoid ACTs. This is because there isn't enough research on how safe they are for early pregnancy. Instead, other medicines like clindamycin and quinine are recommended. For women in their second or third trimesters, ACTs are generally safe.
Some ACTs are avoided for certain groups of people. For example, one combination is not used for newborns. This is because it can make neonatal jaundice worse. Also, some ACTs can cause problems for people with HIV who are taking certain other medicines.
Possible Side Effects
Artemisinin medicines are usually safe when used to treat malaria. The side effects are often similar to malaria symptoms themselves. These can include:
- Feeling sick (nausea)
- Throwing up (vomiting)
- Not wanting to eat
- Feeling dizzy
Sometimes, minor changes in blood tests have been seen. A very rare but serious side effect is an allergic reaction. In one case, a person had serious liver inflammation after taking a high dose of artemisinin for a long time, but they did not have malaria. The other drugs used in combination therapies can also cause side effects. People with acute malaria might experience more side effects from artemisinin drugs.
How Artemisinin Works in the Body
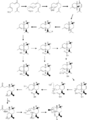
Artemisinin itself is a "prodrug." This means it changes into an active form called dihydroartemisinin (DHA) inside the body. This DHA is the part that actually fights the malaria parasites.
When the drug reaches the malaria parasites inside red blood cells, it reacts with a substance called haem. This reaction breaks open a special ring in the artemisinin molecule. This creates tiny, harmful particles called free radicals. These free radicals then damage important proteins in the parasite, which kills it. Artemisinin is effective against all stages of the malaria parasite's life cycle.
Parasite Resistance
Malaria parasites can sometimes become resistant to medicines. This means the drugs stop working as well. Signs of artemisinin drug resistance were first seen in Southeast Asia in 2008. This resistance has since spread to countries like Cambodia, Thailand, Vietnam, and Myanmar. Scientists have found a specific gene in the parasite that seems to be linked to this resistance.
The WHO is very concerned about resistance to artemisinin. If the parasites become fully resistant, it would be a big problem for fighting malaria worldwide. That's why the WHO pushes for artemisinin to always be used with other anti-malaria drugs. This helps prevent the parasites from developing resistance.
How Artemisinin is Made
Artemisinin can be made in a few ways.
From the Sweet Wormwood Plant
The plant Artemisia annua naturally produces artemisinin. The process involves growing the plant, harvesting its leaves, drying them, and then using a special liquid to pull out the artemisinin.
Making it in Labs and Factories
Scientists have also figured out how to make artemisinin in a lab. They can start with simpler chemicals and build the artemisinin molecule step-by-step. This is called "total synthesis."
Another way is to use engineered organisms. In 2006, scientists at the University of California, Berkeley found a way to change yeast cells. These special yeast cells can produce a part of artemisinin called artemisinic acid. This acid can then be turned into artemisinin. This method is much more efficient than growing the plant. Companies like Sanofi now use this method to produce large amounts of artemisinin. This helps make sure there's enough medicine for everyone who needs it.
Production and Cost
Most of the raw plant material for artemisinin comes from China and Vietnam. Farmers grow the sweet wormwood plants, harvest the leaves, and then the artemisinin is extracted. The price of artemisinin has changed a lot over the years.
Companies like Novartis and Sanofi provide artemisinin combination drugs at a lower cost. This helps make the medicine more affordable for people in need. Scientists are also working to create new types of Artemisia plants that produce more artemisinin. For example, the World Agroforestry Centre developed a hybrid plant called A3. This plant can grow very tall and produce 20 times more artemisinin than wild plants.
However, the WHO does not recommend using A. annua plant materials, like tea made from the leaves, to prevent or treat malaria. This is because the amount of medicine in the tea can vary greatly, and it might not be effective enough.
History of Discovery
The Name Artemisinin
Artemisinin comes from the Chinese name qinghao, which is the sweet wormwood plant. In 1596, a Chinese doctor named Li Shizhen suggested using tea from qinghao to treat malaria symptoms. The plant's name, Artemisia, might come from the Greek goddess Artemis or Queen Artemisia II of Caria, who was a botanist.
Finding the Drug
In 1967, China started a secret military project called "Project 523." Their goal was to find a good treatment for malaria. This was important because many soldiers were getting sick with malaria. In 1972, during this project, Tu Youyou discovered artemisinin in the leaves of Artemisia annua.
Tu Youyou found that a low-temperature method was best for getting the active substance from the plant. She was inspired by an old Chinese medicine book from 340 CE. This book mentioned steeping the herb in cold water. It even gave a recipe: "A handful of qinghao immersed with two litres of water, wring out the juice and drink it all."
Tu's team successfully isolated the substance. Their findings were published in 1979. Artemisinin-based treatments quickly became known as the most effective drugs for malaria. They cleared parasites from patients' bodies faster than other medicines. Project 523 also helped develop other drugs that are now used with artemisinin.
In the late 1990s, the drug company Novartis started making a combination treatment with artemisinin. They offered it at lower prices to the WHO. In 2006, the WHO asked drug makers to stop selling artemisinin by itself. They wanted it only to be sold in combinations with other drugs. This helps stop malaria parasites from becoming resistant.
In 2011, Tu Youyou received a special award for her discovery. Then, on October 5, 2015, she won half of the Nobel Prize in Physiology or Medicine. She was honored for finding artemisinin, a drug that has greatly reduced deaths from malaria.
Future Research
Scientists are always looking for new ways to use artemisinin.
New Combination Therapies
The WHO is looking into other new artemisinin-based combination therapies. These are still in early testing or used only in certain areas.
Fighting Other Parasites
In the 1980s, scientists in China found that artemisinin also works against other parasites. These include flukes, which cause diseases like schistosomiasis. Artemisinin and its related drugs are strong medicines against many types of these worms.
Possible Cancer Treatment
Scientists are also studying if artemisinin and its derivatives could help fight cancer. As of 2018, this research is still in early stages. No artemisinin drugs are approved for treating cancer yet.
Autoimmune Diseases
Artemisinin might also help with diseases where the body's immune system attacks itself, like lupus. One type of artemisinin drug was approved in China in 2015 for testing as a treatment for lupus.
Images for kids
Error: no page names specified (help). In Spanish: Artemisinina para niños
In Spanish: Artemisinina para niños