MRNA vaccine facts for kids
An mRNA vaccine is a special type of vaccine. It uses a copy of a molecule called messenger RNA (mRNA) to teach your body how to fight off germs. Think of mRNA as a tiny instruction manual. The vaccine delivers these mRNA instructions into your immune cells. These cells then use the instructions to build a small part of a germ, like a virus or a cancer cell.
Your body's immune system sees this new protein as foreign. It then learns to identify and destroy the real germ or cancer cells if you ever encounter them. The mRNA is protected and delivered by tiny bubbles called lipid nanoparticles. These bubbles help the mRNA get inside your cells safely.
Like other vaccines, mRNA vaccines can cause some temporary side effects. These are similar to those from traditional vaccines. People with certain immune conditions might react differently. mRNA vaccines have many benefits. They are easy to design and quick to make. They also cost less to produce. They help your body build two types of immunity: cellular and humoral immunity. Plus, they do not change your DNA. Some mRNA vaccines, like the Pfizer–BioNTech COVID-19 vaccine, need very cold storage. Others, like the Moderna COVID-19 vaccine, do not need to be kept so cold.
mRNA vaccines became very important during the COVID-19 pandemic. In December 2020, the Pfizer–BioNTech and Moderna vaccines were approved for use. The UK was the first country to approve an mRNA vaccine. The US Food and Drug Administration (FDA) soon followed.
Contents
How mRNA Vaccines Started
Early Discoveries
Scientists first successfully put designed mRNA into cells in 1989. A year later, they injected unprotected mRNA into mice muscles. These early studies showed that lab-made mRNA could deliver genetic information. This information could then be used to make a desired protein inside living cells. This led to the idea of mRNA vaccines.
In 1993, scientists showed that mRNA inside tiny fat bubbles could make immune cells called T cells react in mice. The next year, they created mRNA that could make copies of itself. This helped mice build strong immunity against a virus. A year later, they showed similar results for fighting cancer cells in mice.
Developing the Technology
The first human trial using mRNA to fight cancer started in 2001. Four years later, scientists found a way to modify mRNA. This helped it get into cells without triggering the body's defense system too much. In 2008, results from a human trial showed an mRNA vaccine directly injected into the body could fight cancer.
Companies like BioNTech (2008) and Moderna (2010) were created to develop mRNA technology. The US research agency DARPA also started investing in this field. They saw the potential of mRNA technology to fight pandemics. This support encouraged other groups to invest too.
The first human trials for an mRNA vaccine against an infectious disease (rabies) began in 2013. In the following years, trials started for other viruses. These included influenza, Zika virus, and Chikungunya virus.
By March 2022, Moderna was working on mRNA vaccines for 15 different diseases. These included Dengue, HIV, Malaria, and Tuberculosis.
Quick Progress with COVID-19
The COVID-19 pandemic began in early 2020. Scientists quickly identified the virus, SARS-CoV-2. This led to the very fast development of the first approved mRNA vaccines. BioNTech and Moderna received approval for their COVID-19 mRNA vaccines in December 2020.
The UK approved the Pfizer–BioNTech vaccine on December 2nd. This was just seven days after its final trial results. It was the first time an mRNA vaccine was approved for widespread use. The US FDA gave emergency approval for the Pfizer–BioNTech vaccine on December 11th. A week later, they approved the Moderna vaccine. Other mRNA vaccines continued to be developed.
How mRNA Vaccines Work
The main goal of any vaccine is to help your adaptive immune system create antibodies. Antibodies are like tiny defense missiles. They are designed to target specific markers on germs, called antigens.
Traditional vaccines work by injecting parts of a germ into your body. These can be antigens, weakened viruses, or dead viruses. Your body then learns to make antibodies against them.
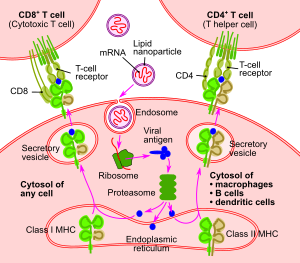
mRNA vaccines work differently. They introduce a small, lab-made piece of the virus's RNA. This RNA piece is quickly taken up by special immune cells called dendritic cells. These cells use their own machinery to read the mRNA instructions. They then produce the viral antigens that the mRNA codes for. Your body gets rid of the mRNA pieces within a few days. The mRNA stays in the cytoplasm of the cell. It does not go into the cell's nucleus where your genomic DNA is stored. So, it cannot change your DNA.
Once the viral antigens are made, your immune system kicks into action. The antigens are broken down. Then, special molecules called MHC molecules grab onto them. They carry the antigens to the cell's surface. This "activates" the dendritic cell. Activated dendritic cells travel to lymph nodes. There, they show the antigens to T cells and B cells. This process triggers your body to make specific antibodies. These antibodies give you immunity against the germ.
What is mRNA in a Vaccine?
The main part of an mRNA vaccine is its mRNA design. This lab-made mRNA is created from a special piece of DNA. Scientists combine this DNA with an enzyme called RNA polymerase. This allows them to make many copies of the mRNA in the lab. How well the vaccine works depends on how stable and well-structured this designed mRNA is.
Lab-made mRNA has the same basic parts as natural mRNA in your cells. It has a 5' cap, a 5'-untranslated region (UTR), a 3'-UTR, and an open reading frame (ORF). The ORF contains the instructions for making the antigen. It also has a 3'-poly(A) tail. Scientists can change these parts of the synthetic mRNA. This makes the mRNA more stable and helps it produce more protein. This, in turn, makes the vaccine work better.
For example, they can use special 5'-cap parts to make the mRNA more stable. They can also change the UTRs and the length of the poly(A) tail. This helps the mRNA last longer and produce more protein. Scientists can also modify the mRNA's building blocks, called nucleotides. This helps reduce unwanted immune reactions and makes the mRNA last longer in the cell. The specific order of the genetic code also affects protein production. Making the mRNA richer in guanine-cytosine helps it stay stable and last longer. Replacing rare genetic codes with common ones also helps make more protein.
How mRNA is Delivered
For a vaccine to work, enough mRNA must get inside your cells. This allows them to make the specific antigens. However, getting mRNA into cells is tricky. mRNA molecules are too big to simply pass through the cell membrane. They also have a negative charge, just like the cell membrane. This causes them to push each other away. Also, mRNA is easily broken down by enzymes in your skin and blood.
Scientists have found different ways to solve these delivery problems. Delivery methods can be divided into two main types: in vivo (inside the body) or ex vivo (outside the body).
Ex vivo Delivery
Dendritic cells are immune cells that show antigens on their surfaces. This helps them interact with T cells to start an immune response. For ex vivo delivery, doctors can collect dendritic cells from a patient. They then program these cells with the desired mRNA in the lab. After that, the programmed cells are put back into the patient. This helps create an immune response.
One way these cells take up mRNA is through a process called endocytosis. This can be made much more efficient in the lab using a method called electroporation.
In vivo Delivery
Since scientists found that injecting lab-made mRNA directly into the body can make antigens, in vivo methods have been explored. These methods have advantages. They avoid the cost and effort of collecting and preparing cells outside the body. They also mimic a natural infection more closely.
Different ways of injecting the vaccine can affect how much mRNA is taken up. For example, injecting into the skin, blood, or muscles can lead to different results. One study showed that injecting into lymph nodes led to the strongest T-cell response.
Polymer and Peptide Carriers
Scientists can mix positively charged polymers with mRNA. This creates protective coatings called polyplexes. These coatings shield the mRNA from enzymes that would break it down. They also help the mRNA get into cells. Protamine, a natural positively charged peptide, has been used to wrap mRNA for vaccines.
Lipid Nanoparticle Carriers
In 2018, the FDA first approved the use of lipid nanoparticles for drug delivery. This was a big step. Putting mRNA inside lipid nanoparticles was a major breakthrough for making effective mRNA vaccines. It solved many problems in getting the mRNA into cells. Research on using lipids to deliver other genetic material helped with this. However, new lipids had to be invented for mRNA. This is because mRNA strands are much longer.
The lipid layer protects the mRNA from breaking down. This allows it to produce more protein. Also, the outer layer of the lipid can be customized. This helps target specific cell types. However, studying this delivery method can be difficult. Results from lab tests do not always match what happens inside a living body. These nanoparticles can be given through different ways, like into a vein or through the lymphatic system.
One challenge with lipid nanoparticles is their production. The special lipids used were made in very small amounts before 2020. They were mainly for research or rare diseases. When mRNA vaccines became important for COVID-19, companies faced a huge challenge. They had to scale up production from grams to tons of these lipids.
Viral Carriers
Besides non-viral methods, scientists have also engineered RNA viruses. These viruses can be used as carriers to achieve similar immune responses. Common RNA viruses used as carriers include retroviruses and alphaviruses. These have been studied in animals like mice and chickens for various diseases.
Benefits of mRNA Vaccines
Over Traditional Vaccines
mRNA vaccines offer special benefits compared to traditional vaccines. Since mRNA vaccines are not made from active or even inactive germs, they cannot cause an infection. Traditional vaccines need to grow germs. Doing this in large amounts could increase the risk of outbreaks at the production facility. Another benefit is that mRNA vaccines make antigens inside your cells. This stimulates both cellular immunity and humoral immunity.
mRNA vaccines can be designed very quickly. Moderna designed their COVID-19 vaccine in just two days. They can also be made faster and more cheaply. The production process is more standardized, meaning fewer errors. This helps respond quickly to serious outbreaks.
The Pfizer–BioNTech vaccine initially took 110 days to mass-produce. This was much faster than traditional flu or polio vaccines. Pfizer later optimized this to 60 days. Within that time, the actual production takes about 22 days. The rest of the time is for strict quality checks at each step.
Over DNA Vaccines
mRNA vaccines also have extra benefits over DNA vaccines. mRNA is used to make proteins in the cytosol (the fluid inside the cell). This means the RNA does not need to enter the cell nucleus. So, there is no risk of it becoming part of your body's genome (DNA).
Scientists can modify the mRNA to reduce unwanted immune reactions. This also helps the mRNA last longer and produce more protein. They can also optimize the mRNA's genetic code. For example, they can increase the guanine-cytosine content. This improves mRNA stability and protein production. An extra genetic instruction can be added to make the mRNA copy itself. This means smaller vaccine doses are needed.
Challenges of mRNA Vaccines
Storage Needs
mRNA is delicate. Some mRNA vaccines must be kept at very low temperatures. This prevents them from breaking down. If they break down, they might not give good immunity. The Pfizer–BioNTech mRNA vaccine needs to be stored between -80 and -60 degrees Celsius (-112 and -76 degrees Fahrenheit). Moderna says their vaccine can be stored between -25 and -15 degrees Celsius (-13 and 5 degrees Fahrenheit). This is like a home freezer. It can also stay stable for up to 30 days between 2 and 8 degrees Celsius (36 and 46 degrees Fahrenheit). Scientists are working on ways to store them at higher temperatures.
New Technology
Before 2020, no mRNA technology (drug or vaccine) had been approved for human use. This meant there was a risk of unknown effects. The COVID-19 pandemic pushed for faster production of mRNA vaccines. This made them attractive to health organizations. It also led to discussions about how quickly they should be approved.
Side Effects
Side effects from mRNA vaccines are similar to those from traditional vaccines. However, people prone to autoimmune reactions might react differently. The mRNA in the vaccine might cause an unintended immune reaction. This can make a person feel like they are sick. To reduce this, mRNA sequences in vaccines are designed to mimic those made by your own cells.
Strong but temporary side effects were reported in COVID-19 mRNA vaccine trials. Most people will not have severe side effects, which include fever and tiredness. Severe side effects are those that stop you from doing daily activities.
How Well Do They Work?
The COVID-19 mRNA vaccines from Moderna and Pfizer–BioNTech have very high effectiveness rates, around 90 to 95 percent. Before this, some mRNA drug trials for other germs were not effective. They had to be stopped early. The exact reason for the high effectiveness of the new mRNA vaccines is not fully clear.
Some scientists suggest the high effectiveness might be due to the huge amount of resources put into their development. Another idea is that the vaccines might cause a general immune response to the mRNA itself. This could boost the specific immune response. This might also explain the strong reactions like aches and fevers reported by some people. These reactions were temporary. Another view is that these reactions were due to the lipid delivery molecules.
Understanding mRNA Vaccines
There has been false information suggesting that mRNA vaccines could change your DNA. This is not true. mRNA in the cell's cytosol breaks down very quickly. It does not have time to enter the cell nucleus where your DNA is. In fact, mRNA vaccines must be stored at very low temperatures. They also need to be kept away from enzymes that break down RNA. This is to prevent the mRNA from degrading.
Some viruses, called retroviruses, have RNA that can enter the cell nucleus. They use a special enzyme to make DNA from their RNA. However, a retrovirus has specific ways to get into the nucleus. Other mRNA, like that in a vaccine, does not have these ways. Even if vaccine mRNA could enter the nucleus, it would need special enzymes and tools to make DNA from RNA. These are only present with a retrovirus, not with vaccine mRNA.
Types of mRNA Vaccines
mRNA vaccines use either non-amplifying (regular) mRNA or self-amplifying mRNA. The Pfizer–BioNTech and Moderna vaccines use non-amplifying mRNA. Both types of mRNA are still being studied for vaccines against other germs and cancer.
Non-amplifying mRNA
The first mRNA vaccines use non-amplifying mRNA. This type of mRNA has only one set of instructions. These instructions code for the antigen of interest. The amount of mRNA available to the cell is equal to the amount delivered by the vaccine. The vaccine dose is limited by how much mRNA can be delivered. Non-amplifying vaccines often replace a building block called uridine with N1-Methylpseudouridine. This helps reduce unwanted side effects.
Self-amplifying mRNA
Self-amplifying mRNA (saRNA) vaccines make copies of their mRNA after they enter the cell. Self-amplifying mRNA has two sets of instructions. The first set codes for the antigen, like regular mRNA. The second set codes for an enzyme that copies the mRNA inside the cell. This means smaller vaccine doses can be used. Self-amplifying mRNA is a much larger molecule. So, how it works and how it is evaluated might be different.
SaRNA vaccines are being researched for diseases like Malaria. In 2021, a company started a trial for an saRNA COVID-19 vaccine. This vaccine is designed to be a booster vaccine. It targets both the main part of the virus and other viral proteins. This aims to give better protection against different virus versions. SaRNA vaccines must use uridine, which is needed for the copying process.
See also
 In Spanish: Vacuna de ARN para niños
In Spanish: Vacuna de ARN para niños
- DNA vaccine
- Nucleoside-modified messenger RNA
- RNA therapeutics
- Timeline of human vaccines
 | Claudette Colvin |
 | Myrlie Evers-Williams |
 | Alberta Odell Jones |