Osteoblast facts for kids
Quick facts for kids Osteoblast |
|
|---|---|
 |
|
|
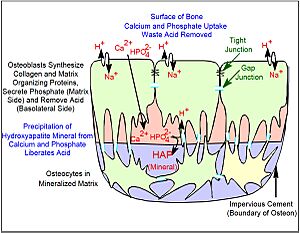
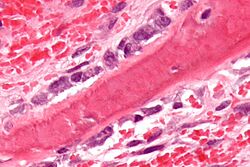
Osteoblasts (purple) are cells that help build bone. They are shown here next to a piece of bone (pink).
|
|
 |
|
| An illustration of a single osteoblast cell. |
Osteoblasts are special cells that build new bone. The word "osteoblast" comes from Greek words meaning "bone" and "to grow." These cells work together in groups to make bone. One single osteoblast cannot make bone by itself. A group of osteoblasts working together, along with the bone they create, is often called an osteon.
Osteoblasts come from special "master cells" called mesenchymal stem cells. They create a strong, flexible material called collagen. They also make smaller amounts of other important proteins like osteocalcin and osteopontin. These proteins form the basic structure of bone.
After making the basic structure, osteoblasts add hydroxyapatite, which is the main bone mineral. This mineral is carefully placed into the bone structure, making it very strong and dense. Our skeleton is mostly made of this strong, mineralized bone. It supports our bodies and also stores important minerals like calcium and phosphate. These minerals are vital for keeping our body's chemistry balanced.
Contents
How Bones Are Built and Changed
Our skeleton is a living organ that is always changing. It's built up and broken down throughout our lives. The skeleton is important for supporting our body. It also helps keep the right levels of calcium, phosphate, and acid in our body.
The main part of bone is called the bone matrix. This matrix is outside the cells. It's made of protein and mineral. The protein part is called the organic matrix. It's made first, and then the mineral is added. Most of the organic matrix is collagen. Collagen gives bone its ability to stretch and bend without breaking.
The matrix is made hard by adding hydroxyapatite mineral. This mineral is very hard and gives bone its strength to resist being crushed. So, collagen and mineral together make a super strong material. It can bend a little and then return to its original shape. This is called elastic deformation. If too much force is put on a bone, it can break. This is called a bone fracture.
Osteoblasts: The Bone Builders
Osteoblasts are the main cells that make up bone. They come from mesenchymal stem cells (MSCs). MSCs can also turn into fat cells or muscle cells. Osteoblasts are found in large numbers in the periosteum. This is a thin layer of tissue on the outside of bones. They are also found in the endosteum, which lines the inside of bones.
Before the bone matrix becomes hard with minerals, it's called osteoid. Osteoblasts that get surrounded by the new bone matrix are called osteocytes. When osteoblasts are actively building bone, they look like small cubes. When they are not actively building bone, they become flat and are called inactive osteoblasts. Osteocytes stay alive and are connected to the surface osteoblasts. They play an important role in keeping our bones healthy.
Osteoclasts: The Bone Removers
Osteoclasts are large cells with many nuclei. They come from cells in the bone marrow that also make white blood cells. Osteoclasts break down bone tissue. They work with osteoblasts and osteocytes to keep bone healthy.
Inside our bones, there are many other types of cells in the bone marrow. For osteoblasts to build bone, they need mesenchymal stem cells (which become osteoblasts). They also need blood vessels to bring oxygen and nutrients. Bone is a tissue with lots of blood vessels. New blood vessels are always forming to support bone activity.
As people get older, especially women after menopause, the balance between bone building and bone breaking down can change. More bone might be broken down than built. This can lead to a condition called osteoporosis, where bones become weak and can break easily.
How Bones Develop
Bone is formed in two main ways: endochondral ossification or intramembranous ossification.
- Endochondral ossification is the most common way. It's how most of our bones form. First, a model of the bone is made from cartilage by cells called chondrocytes. Then, this cartilage is removed and replaced by bone made by osteoblasts.
- Intramembranous ossification is when bone forms directly from a type of tissue called mesenchyme. This happens when bones like those in our skull are formed.
During the development of osteoblasts, certain special proteins called transcription factors are important. These include Cbfa1/Runx2 and Sp7. These factors help guide the cells to become osteoblasts. Osteoblasts can also form in a lab if they have the right conditions, like vitamin C and certain enzymes.
Special Proteins for Bone Growth
Special proteins called bone morphogenetic proteins (BMPs) are very important for bone development. They help decide where cartilage forms and where spaces are left between bones. Another important protein family is Transforming growth factor beta (TGF-β). It helps cartilage develop, which is often the first step before bone forms. Fibroblast growth factors (FGFs) also help decide where bone parts appear in relation to the skin.
Hormones and Bone Health
Many other systems help control the change from cartilage to bone and keep bones healthy. A very important hormone for bones is parathyroid hormone (PTH). PTH is made by the parathyroid gland and helps control the amount of calcium in our blood. PTH can help increase osteoblast activity, but too much PTH can also cause bone to break down.
Our bones also change based on our diet and other hormones. For example, estrogen and glucocorticoids (steroids) affect bone. These hormones are important for reproduction and how our body uses energy. Building and breaking down bone uses a lot of energy. Other hormones from the pituitary gland, like adrenocorticotropic hormone (ACTH) and follicle stimulating hormone, also play a role, though we are still learning exactly how they work with bone.
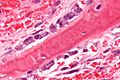
How Osteoblasts Connect
When we look at bone very closely with a powerful microscope, we can see that individual osteoblasts are connected. They have tight junctions that prevent fluid from passing through. This creates a special "bone compartment" that is separate from the general fluid around cells.
Osteoblasts are also connected by gap junctions. These are tiny pores that link osteoblasts together. This allows the cells in one group to work as a single unit. These gap junctions also connect deeper cells (osteocytes) to the surface osteoblasts. This means that all the cells in a bone-forming unit can communicate and work together. Bone is made of many of these units, which are separated by areas with no cell connections.
Collagen and Other Bone Proteins
Most of the non-mineral part of bone is made of strong collagen type I. This collagen forms dense, interwoven ropes that give bone its ability to resist pulling forces. Osteoblasts lay down layers of collagen in a very organized way. Some layers run along the length of the bone, and others are at right angles.
Small but important amounts of other proteins are also found in bone. These include osteocalcin and osteopontin. Osteocalcin is mostly found in bone, so it's a good sign that new bone is being made. These proteins help connect the mineral and collagen parts of the bone, making it as strong as possible.
Bone Versus Cartilage
Our early skeleton is made of cartilage. Cartilage is a solid tissue without blood vessels. It contains cells called chondrocytes, which make the cartilage matrix. Unlike osteoblasts, chondrocytes don't have connections between them and don't work in coordinated units. Cartilage is made of a network of collagen type II and water-absorbing proteins. This is what the adult skeleton of sharks is made of. It's also the first skeleton that forms in more advanced animals.
In animals that breathe air, cartilage is replaced by bone. Sometimes, cartilage first becomes mineralized. This mineralized cartilage is not very dense or strong. It acts as a temporary structure for osteoblasts to build new bone on. Then, osteoclasts remove this mineralized cartilage.
Osteoblasts create a more advanced type of bone matrix. It has dense, irregular crystals of hydroxyapatite packed around the collagen ropes. This creates a very strong material. This allows long bones to be shaped like hollow tubes. Making them hollow reduces weight while keeping them strong.
How Bone Gets Its Minerals
Scientists are still learning exactly how bone gets its minerals. When certain fluorescent dyes are given for a short time, they stick strongly to new bone mineral. They show up as narrow bands in the new bone. These bands appear where osteoblasts are actively forming bone. This suggests that osteoblasts actively transport minerals to build bone. It's not just minerals from our diet passively forming bone.
The way bone gets its minerals is different from how cartilage gets mineralized. In cartilage, minerals spread throughout the tissue. But in bone, osteoblasts create a special, sealed space where minerals are deposited. This is because the osteoblasts are connected by tight junctions. This means phosphate and calcium can't just move in and out freely.
Calcium is moved across osteoblasts by special transporters. Phosphate is actively produced by osteoblasts. They release phosphate-containing compounds and use enzymes called phosphatases to create a high concentration of phosphate where minerals are deposited. Alkaline phosphatase is a key enzyme found on active osteoblasts.
When minerals are deposited, acid is produced. In a closed system, this acid would stop more minerals from forming. But osteoblasts have ways to remove this acid, allowing bone formation to continue.
Osteocyte Feedback
Our bones respond to physical activity. Being active helps maintain bone mass. Also, osteocytes (the osteoblasts trapped in bone) send signals that limit how big a bone-forming unit can get. Osteocytes release a protein called sclerostin. This protein stops a process that keeps osteoblasts active. So, when a bone-forming unit reaches a certain size, it stops making new bone.
See also
- List of human cell types derived from the germ layers
- List of distinct cell types in the adult human body
Images for kids
 | Tommie Smith |
 | Simone Manuel |
 | Shani Davis |
 | Simone Biles |
 | Alice Coachman |