Moraxella catarrhalis facts for kids
Quick facts for kids Moraxella catarrhalis |
|
|---|---|
 |
|
| Scientific classification |
|
| Domain: | Bacteria |
| Phylum: | Proteobacteria |
| Class: | Gammaproteobacteria |
| Order: | Pseudomonadales |
| Family: | Moraxellaceae |
| Genus: | Moraxella |
| Species: |
M. catarrhalis
|
| Binomial name | |
| Moraxella catarrhalis (Frosch and Kolle 1896) Henriksen and Bøvre 1968
|
|
| Script error: The function "autoWithCaption" does not exist. | |
Script error: No such module "Check for conflicting parameters".
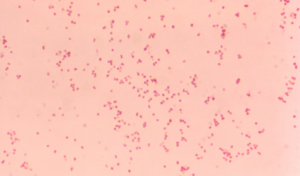
Moraxella catarrhalis is a tiny germ, a type of bacteria, that can cause infections in people. It's a bit picky about where it grows (fastidious). It doesn't move on its own (nonmotile). This germ is Gram-negative, which is how scientists classify bacteria. It needs air to live (aerobic) and gives a positive result in an oxidase test. It looks like two tiny round cells joined together (a diplococcus).
This bacterium can cause problems in your respiratory system (like your lungs and throat), middle ear, eyes, central nervous system (brain and spinal cord), and joints. It causes infection by sticking to your body's cells using special proteins.
Contents
Where It's Found
Moraxella catarrhalis mainly lives in the upper breathing passages of humans. It can also infect other animals, like macaques, which are a type of monkey.
Its Name Story
This bacterium used to have a different name, Branhamella. Scientists changed its name to Moraxella catarrhalis after looking closely at its DNA and other tiny parts. They found it was more like other bacteria in the Moraxella group. Even so, some doctors still use the old name sometimes.
The name Moraxella comes from Victor Morax. He was a Swiss eye doctor who first described these types of bacteria. Catarrhalis comes from an old Greek word meaning "to flow down." This describes the runny nose and eyes you often get with a bad cold.
Its Genetic Code
Scientists have fully mapped out the genetic code, or genome, of M. catarrhalis. This information was made public in 2016. It helps researchers understand the bacterium better.
What Infections It Causes
This bacterium is known to cause several common infections. These include otitis media (ear infections), bronchitis (chest colds), sinusitis (sinus infections), and laryngitis (sore throat with voice loss).
Older people and heavy smokers with chronic obstructive pulmonary disease (COPD) can get serious lung infections like bronchopneumonia from M. catarrhalis. It can also make their existing lung problems worse.
Young children, especially around age two, are very likely to carry this bacterium. As people get older, it becomes much less common to have it in their bodies.
Moraxella catarrhalis is now seen as an important germ that can cause illness. It can lead to lung infections, especially in people with weaker immune systems. It can also cause bacterial pneumonia. It often makes chronic lung diseases worse. This bacterium can also cause acute sinusitis, eye infections (conjunctivitis), and ear infections in children. Rarely, it can cause more serious problems like sepsis (a severe body reaction to infection) or septic arthritis (joint infection). M. catarrhalis often attacks people who are already sick or have weak immune systems.
When It Enters the Bloodstream
Moraxella catarrhalis has been linked to septic arthritis when it gets into the bloodstream. This is called bacteremia. While rare, cases of M. catarrhalis causing bloodstream infections have been reported. Sometimes, these infections can be serious, causing fever or even sepsis.
If a lot of these bacteria get into the bloodstream, it can sometimes lead to endocarditis. This is an infection of the heart lining. Doctors used to miss M. catarrhalis infections because it was only recently (in the 1990s) recognized as a major cause of illness. People with other health problems or weak immune systems are more likely to get severe bloodstream infections from this bacterium.
Fighting Back: Antibiotic Resistance
Doctors can treat Moraxella catarrhalis infections with antibiotics. However, this bacterium is often resistant to common antibiotics like penicillin, ampicillin, and amoxicillin. This means those medicines might not work.
Scientists are working hard to find a good vaccine for M. catarrhalis. They are also trying to understand how it causes disease. For example, they are studying how it resists the body's natural defenses.
Many strains of M. catarrhalis are resistant to ampicillin and amoxicillin. This is because they produce special proteins called beta-lactamases. These proteins break down the antibiotics, making them useless. These beta-lactamases can even help other bacteria nearby become resistant to antibiotics.
Researchers have found a large protein on the surface of M. catarrhalis called UspA. This protein could be a target for new medicines or vaccinations. If our bodies can make antibodies against UspA, they might be able to fight off the infection.
Studies in mice have shown that giving them a vaccine for M. catarrhalis helps their bodies fight the infection better. This means that antibodies in the blood play a big role in protecting the lungs. Scientists believe that certain proteins on the outside of the bacterium could be used to create a vaccine.
How Infections Are Treated
Treatment for M. catarrhalis infections usually involves antibiotics. Sometimes, doctors might suggest a "watchful waiting" approach, especially for mild ear infections. This means they wait to see if the body can fight off the infection on its own.
Because most M. catarrhalis strains are resistant to penicillin, doctors often use other antibiotics. These include fluoroquinolones, some types of cephalosporins, erythromycin, and amoxicillin-clavulanate.
Developing a Vaccine
Right now, there isn't a widely available vaccine in the US for M. catarrhalis infections. However, because it causes many breathing problems, scientists are actively trying to develop one. They are looking at different proteins on the bacterium's outer surface as possible targets for a vaccine.
How It Looks and Works
When scientists grow M. catarrhalis in a lab, they see it as a large, kidney-shaped, Gram-negative diplococcus. It grows well on special plates called blood and chocolate agar if kept warm (37°C) for 24 hours with air. The colonies look like gray-white domes, about 1 millimeter wide. They are fragile and crumble easily, with a waxy surface.
A fun test called the "hockey puck test" is used. If you can slide the colonies across the plate with a stick, it's a positive result, which M. catarrhalis does. These bacteria don't break down red blood cells (no hemolysis). They also don't ferment sugars like glucose or lactose. However, they can produce DNase and give positive results for oxidase, lipase, and nitrate reduction. These tests help labs quickly identify M. catarrhalis.
Scientists have studied the outer proteins of M. catarrhalis strains. They found that these proteins are very similar across different strains. This similarity is good news for vaccine development. One specific protein, called an 80-kDa OMP, is found in all non-covered strains. This makes it a good candidate for a vaccine.
How Proteins Move Inside the Bacterium
Moraxella catarrhalis has a special system called the twin-arginine translocation pathway (TAT pathway). This pathway helps move important folded proteins across the bacterium's inner membrane. It uses three main proteins: TatA, TatB, and TatC. TatA forms a tiny hole, and TatB and TatC help guide the proteins to this hole.
The genes for these Tat proteins are found together in the bacterium's DNA. Many proteins in M. catarrhalis are thought to use this TAT pathway. For example, the beta-lactamase proteins (which cause antibiotic resistance) are moved this way. This pathway is important for M. catarrhalis to grow well, even without antibiotics around.


