Health equity facts for kids
Health equity means that everyone has a fair chance to be as healthy as possible. It's about making sure everyone has what they need to be healthy. This includes things like good food, safe places to live, and access to doctors. It's not just giving everyone the same things; that's called equality. Instead, health equity means giving people what they *need* to reach the same level of health.
The World Health Organization says health is about feeling good physically, mentally, and socially, not just not being sick. How healthy people are in a country, and how health is shared among different groups, shows how developed that country is. Being healthy is a basic human right.
The CDC says health equity is "the state in which everyone has a fair and just opportunity to attain their highest level of health." It's linked to the idea of social justice, where good health is a basic right for everyone. Health differences can be seen in how often people get sick, their health results, or how easily they can get healthcare. These differences can be based on a person's race, ethnicity, gender, disability, or socioeconomic status (how much money and education they have).
Health inequity is different from health inequality. Health inequality means there are differences in health between groups, even if they have similar access to healthcare. But health inequity means these differences are unfair, avoidable, and unjust. They can't be explained by natural things like genetics or personal choices. For example, if one group lives shorter lives because of their genes, that's an inequality. But if they live shorter lives because they can't get medicine, that's an inequity. Getting fair access to healthcare is very important for reaching many global goals for development.
Contents
Money and Health
How much money and education a person has (their socioeconomic status) is a big sign of how healthy they will be. It's also a main reason for health differences between groups. Not having enough money can really limit what a person or group can do. This includes not having enough money or social connections. It's easy to see how not having enough money can make it hard to stay healthy. Income affects whether you can get healthcare. Your job is a main way to get money and social connections. So, work is an important factor in health differences.
A job can affect your health in many ways. This includes how physically demanding it is, if you're around dangers, how you're employed, your pay and benefits, and if there are health and safety programs. People with steady jobs are less likely to be poor. They are also more likely to have healthcare. Staying healthy with proper healthcare can be very expensive. This makes it hard for some people to afford.
For example, in China, a healthcare system called the Cooperative Medical System broke down. This left many poor people in the countryside without health insurance. They couldn't get the care they needed to stay healthy. Medical costs went up, making healthcare even harder to afford. This problem got worse because the gap between rich and poor people in China grew. Poor Chinese people often couldn't go to the hospital when needed. They also couldn't finish their treatments. This led to worse health.
In Tanzania, studies showed that richer families were much more likely to take their children to a doctor. This is a big step towards better healthcare. Unequal income itself can make a society less healthy. This happens because there's less money invested in public services like education and healthcare. It also breaks down community connections.
Social connections are also very important for health. People who are better connected to others in their community tend to live longer. Communities are often separated by income all over the world. This greatly affects health quality. It means people in poor neighborhoods have fewer social connections. Programs that try to improve healthcare by boosting a community's social resources are good ways to make people healthier.
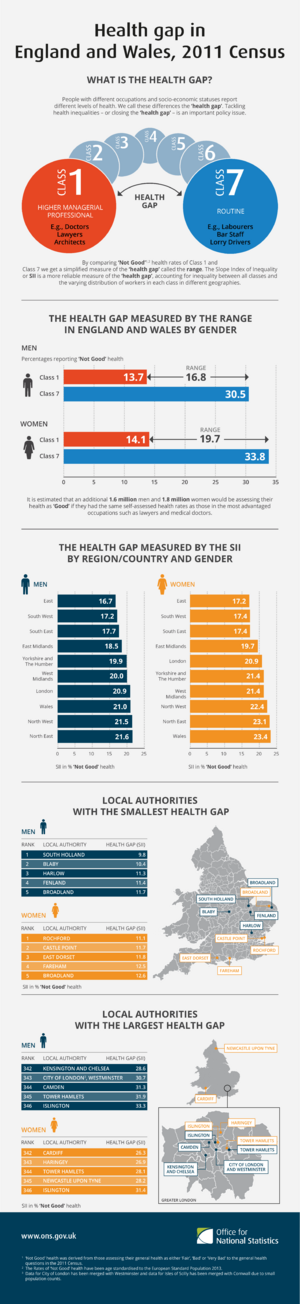
How Money Differences Affect Health
Poor health seems to be a result of big differences in money across a population. Countries and regions with bigger gaps between rich and poor often have worse health. This includes shorter lives, more mental health issues, more obesity, lower school performance, and more illness from violence. Around the world, rich countries with more equal wealth tend to have longer lifespans. This is true no matter how much money the average person makes in those rich countries. Money only greatly affects how long people live in countries where the average yearly income is less than about $25,000.
The United States has surprisingly poor health results for a developed country. This is true even though it spends the most money on healthcare in the world. The U.S. ranks 31st in how long people live. Americans live shorter lives than people in Europe. This is true even when you compare people with similar race, income, diet, smoking habits, and education.
Differences in wealth negatively affect health at global, national, and local levels. The same patterns seen worldwide are true between states in the U.S. that are more or less equal in wealth. States with more equal wealth show better health results. Importantly, inequality can hurt the health of people at lower levels within organizations. Studies like the Whitehall Study looked at heart disease in British government workers. They found that even with similar lifestyles, people with lower status in their jobs had higher rates of illness and death. This was a steady decline from those with higher status.
The bad effects of inequality spread across the whole population. For example, comparing the U.S. (a less equal nation) to England (a more equal nation), the U.S. has higher rates of diabetes, high blood pressure, cancer, lung disease, and heart disease at *all* income levels. This is also true when comparing very equal Sweden to less equal England.
Giving money directly to poor people in some developing countries seems to make them less likely to get sick. This shows that such help can be a good way to use resources.
The quality of healthcare changes among different income groups. Children in poor families are most likely to face health differences. Young children (under 5) in poor families often have health problems. This is because their health depends on others taking care of them. They can't stay healthy on their own. Also, these children have higher death rates than richer children because of poor food. Because they are poor, getting healthcare can be hard. Children in poor families are less likely to get healthcare. If they do, the care might not be very good.
Education and Health
Education is important for using healthcare, but it's also linked to how much money you have. A person might not go to a doctor or seek care if they don't know why it's important. They might not understand the value of proper treatment.
In Tajikistan, since the country became independent, more women with less education have given birth at home. Education also greatly affects the quality of care mothers get before and after birth. Mothers with only a basic education saw a doctor during pregnancy much less often (72%) than those with more education (77% for secondary, 88% for technical, and 100% for higher education). There's also a link between income and health knowledge. One study showed that richer Tanzanian families were more likely to spot diseases in their children than poorer families.
Social unfairness is a big block to getting health information. Patients in poorer areas have less access to health information in general. This means they know less about different diseases and health issues. Health education has been shown to be a strong way to prevent illness and encourage people to see doctors. Not having health education can lead to worse health in these areas.
Differences in education are also closely linked to health differences. People with less education are more likely to have greater health risks. Education is also linked to better understanding of health information and services. This helps people make good health choices. It's also linked to living longer. Students with good grades tend to have better health habits and fewer risky behaviors than those who don't do as well in school. Things like poor diets, not enough exercise, and physical or emotional abuse greatly affect how well students do in school. These problems happen more often to people with lower incomes.
Health Differences by Location
For some people, getting to healthcare and health resources is physically hard. This leads to health differences. For example, a person might not be able to travel the long distances needed to reach doctors. Or, long distances might make regular care seem not worth the effort, even if it would help.
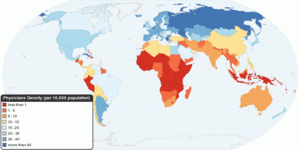
In 2019, the U.S. government said that almost 80% of rural America was "medically underserved." This means these areas lacked skilled nursing homes, rehabilitation centers, mental health units, and intensive care units. In rural areas, there are about 68 primary care doctors for every 100,000 people. In cities, there are 84 doctors for every 100,000 people. According to the National Rural Health Association, almost 10% of rural counties had no doctors in 2017. Rural communities have shorter lives and higher rates of diabetes, long-term illnesses, and obesity.
Costa Rica, for example, has clear health differences based on location. About 12–14% of the people live in areas where healthcare is hard to reach. These differences have decreased in some parts of the country because of healthcare reform programs. However, areas not helped by these programs have seen a slight increase in health differences.
China saw a big drop in fair health access by location after its economic changes in the 1980s. This happened because the Cooperative Medical System (CMS) got worse. The CMS had provided healthcare in rural areas. It also had a way to get money from communities and government help. Without it, there was a big drop in the number of healthcare workers (35.9%) and working clinics (from 71% to 55% of villages over 14 years) in rural areas. This led to unfair healthcare for people in the countryside. The severe poverty of rural workers (some earning less than US$1 per day) further limits access to healthcare. It also causes poor food and hygiene. This makes the loss of healthcare resources even worse. The loss of the CMS has clearly affected how long people live. Rural areas, like parts of Western China, have much shorter life expectancies.
Similarly, people in rural Tajikistan face health differences based on where they live. A study by Jane Falkingham found that being able to physically get to healthcare was one of the main things affecting the quality of care for mothers. Also, many women in rural areas of the country didn't have enough access to healthcare. This led to poor care for mothers and newborns. For example, these rural women were much more likely to give birth at home without medical help.
Differences by Race and Ethnicity
Besides money, race is another key factor in health differences. The United States has historically had big differences in health and access to good healthcare between races. Current information shows that these race-based differences still exist. They are a serious social health problem. These differences include how good the care is based on race, and how many people have health insurance based on race. A 2002 study found that race greatly affects the quality of care. Black people received lower quality care than white people. This is partly because many ethnic minorities, like African Americans, earn low incomes or live in poverty. In 2007, African American families made an average of $33,916, while white families made $54,920. Because of a lack of affordable healthcare, African Americans have a higher death rate from causes that could have been treated or prevented.
For example, a 2005 study found that African American men were 30% more likely to die from heart disease than white men. African American women were 34% more likely to die from breast cancer than white women. Also, death rates for African American and Latino babies are 2 to 3 times higher than for other racial groups. A study of over 2 million pregnancies found that babies born to Black women worldwide had worse outcomes (like baby death or stillbirth) than babies born to White women. This was true even when considering older mothers or those with less education (which can mean poorer economic status). In the same study, Hispanic women were 3 times more likely to experience a baby death than White women. South Asian women had a higher risk of early birth and having a baby with low birthweight compared to White women.
These differences also greatly affect indigenous communities. As people in indigenous communities adopt Western ways of life, they become more likely to get certain long-term illnesses.
There are also big racial differences in who has health insurance. Ethnic minorities generally have less insurance than non-ethnic minorities. For example, Hispanic Americans tend to have less insurance than white Americans. Because of this, they get less regular medical care. Having health insurance is directly linked to getting healthcare, including check-ups and basic care. A 2010 study found that these differences cannot be fully explained by things like insurance status, income, education, age, or where people live. Even when researchers adjusted for these factors, the differences remained. Slavery has led to different health outcomes for generations of African Americans in the United States.
Ethnic health differences also appear in countries across Africa. A 2000 study looked at child deaths in 11 African nations. It found big ethnic differences in death rates for children under 5, as well as in education and vaccine use. In South Africa, the history of apartheid still means different access to social services, including healthcare, based on race and social class. This leads to health differences. Also, there's evidence that indigenous people are often ignored in many countries. For example, the Pygmies of Congo are left out of government health programs. They face discrimination during public health campaigns and get poorer overall healthcare.
A 1995 study in five European countries (Sweden, Switzerland, the UK, Italy, and France) found that only Sweden provided translators for 100% of those who needed them. Other countries lacked this service. This could hurt the healthcare of people who don't speak the local language. Since non-native people made up a good part of these countries (6%, 17%, 3%, 1%, and 6% respectively), this could have serious bad effects on health fairness. In France, an older study noted big differences in healthcare access between native French people and non-French/migrant people. This was based on how much they spent on health. However, this was also linked to poorer economic and working conditions for these groups.
A 1996 study of race-based health unfairness in Australia showed that Aborigines had higher death rates than non-Aborigine people. Aborigine people had 10 times higher death rates in the 30–40 age range. They also had 2.5 times higher infant death rates and 3 times higher age-adjusted death rates. Rates of diarrhea and tuberculosis were also much higher in this group (16 and 15 times greater, respectively). This shows the poor healthcare for this ethnic group. At that time, the differences in how long people lived at birth between indigenous and non-indigenous people were highest in Australia, compared to the U.S., Canada, and New Zealand. In South America, indigenous people faced similarly poor health. Their rates of mothers and babies dying were much higher (up to 3 to 4 times greater) than the national average. The same pattern of poor indigenous healthcare continues in India. Indigenous groups there showed higher death rates at most stages of life, even when considering environmental effects.
Because of unfair health and social systems, people from racial and ethnic minority groups in the United States are affected more by COVID-19.
On February 5, 2021, the head of the World Health Organization (WHO), Tedros Adhanom Ghebreyesus, spoke about the unfair global access to COVID-19 vaccines. He noted that almost 130 countries had not given a single dose yet. In early April 2021, the WHO reported that 87% of vaccines had gone to the richest countries. Only 0.2% had gone to the poorest countries. As a result, one-quarter of the people in wealthy countries had already been vaccinated. But only 1 in 500 people in poor countries had received a vaccine.
Sex and Gender in Healthcare
Both gender and sex are important factors that affect health. Sex refers to biological differences between males and females, like genes, hormones, and body parts. Gender is about how a person acts and lives their life. Both sex and gender affect each other. Differences between genders influence how diseases show up and how healthcare is given. Understanding how sex and gender work together helps doctors give good care to patients. It can be hard to tell the difference between sex and gender because they are so connected. Both can cause health differences. They both make people more likely to get certain health problems, like heart disease and autoimmune disorders.
Health for Males
Gender and sex both play a role in health differences for males. In some non-Western areas, males tend to have better health than women because of gender discrimination. In most parts of the world, more adult men die than adult women. For example, adult men get deadly illnesses more often than females. The main reasons for higher male death rates are accidents, injuries, violence, and heart diseases. In most parts of the world, violence and traffic accidents cause most deaths in teenage boys.
Health for Females
Gender and sex also play a role in health differences for females. The 2012 World Development Report noted that women in developing nations die more often than men in those countries. Also, women in developing countries have a much higher risk of maternal death (dying during childbirth) than those in developed countries. The highest risk of dying during childbirth is 1 in 6 in Afghanistan and Sierra Leone. This is very different from nearly 1 in 30,000 in Sweden. This difference is much bigger than for newborn or child mortality.
While women in the United States tend to live longer than men, they often have lower socioeconomic status (SES). This means they face more barriers to getting healthcare. Having lower SES can also increase social pressures. This can lead to higher rates of depression and long-term stress. These, in turn, can hurt health. In Europe, women who grew up poor are more likely to have weaker muscles and more disabilities when they are old. Women in the U.S. have better access to healthcare than in many other places. But having enough health insurance to pay for care, like for after childbirth, can help avoid extra hospital visits.
In one study in Harlem, New York, 86% of women said they had private or public health insurance. Only 74% of men reported having any health insurance. This is similar to the general population in the U.S. On the other hand, women's access to healthcare in rural communities has become a worry. Access to care for mothers giving birth has gone down in rural areas. This is because more hospitals and birth centers have closed. This puts a bigger burden on families in these areas. Women in these rural communities face financial burdens from traveling to get good care. Millions of people in rural U.S. areas are more at risk of having less access to care for mothers if their community is low-income. These women are more likely to have bad outcomes for mothers, like a higher risk of postpartum depression, giving birth outside a hospital, and, in serious cases, death or severe illness for the mother.
Also, women's pain tends to be taken less seriously and ignored by doctors at first, compared to men's pain complaints. Historically, women were not included in the design of clinical trials. This slowed down understanding how women react to medicines. It created a gap in research. This has led to bad side effects in women after drugs were approved. Several drugs have even been removed from the market. However, the research industry knows about this problem and is working to fix it.
Cultural Factors in Health
Health differences are also partly due to cultural factors. These involve practices based on sex and gender roles. For example, in China, health differences have led to different medical treatment for men and women. This is because of a cultural preference for male children. Recently, gender-based differences have decreased as females have started to receive better care.
In India, gender-based health differences are clear in early childhood. Many families give better food to boys. This is because boys are often seen as future earners for the family. Also, boys receive better care than girls and are hospitalized more often. These differences get bigger the more poverty there is in a group.
Environmental Effects on Health
Minority groups are more exposed to environmental dangers. These include a lack of neighborhood resources, community problems, and living in separated areas. This can lead to a cycle of illness and stress. Our surroundings can affect our choices and lead to poor health. Minority neighborhoods often have more fast-food restaurants and fewer grocery stores than mostly white neighborhoods. These "food deserts" make it hard for families to get healthy food for their children. This lack of healthy food goes beyond homes into schools. Schools often have many vending machines and serve overly processed foods. These environmental conditions have social effects. For the first time in U.S. history, it's predicted that the current generation will live shorter lives than their parents.
Also, minority neighborhoods have various health dangers. These come from living near highways and toxic waste factories, or in run-down buildings and streets. These environmental conditions create different levels of health risk. This includes noise pollution and cancer-causing toxic exposures from asbestos and radon. These lead to more long-term illnesses, sickness, and deaths. The quality of where people live, like damaged housing, has been shown to increase the risk of bad birth outcomes. This shows a community's health. This happens through exposure to lead in paint and soil, as well as indoor air pollution like secondhand smoke and tiny particles. Housing conditions can create different health risks. These lead to birth problems and long-term issues for older people.
Also, job dangers can add to the bad effects of poor housing. More minority people work in jobs with higher exposure to toxic chemicals, dust, and fumes. One example is the environmental dangers that poor Latino farmworkers face in the United States. This group is exposed to high levels of particles and pesticides at work. This has led to more cancer, lung problems, and birth defects in their communities.
Racial separation is another environmental factor. It happens because of unfair actions by real estate companies and people working in housing or rentals. Even though living separation is seen in all minority groups, Black people tend to be separated no matter their income, compared to Latinos and Asians. So, separation causes minorities to live in poor neighborhoods. These areas have limited jobs, medical care, and education. They are also linked to high rates of crime. Also, separation affects the health of people living there. This is because the environment is not good for exercise. Neighborhoods might be unsafe, lack sports facilities, and have no park space. Racial and ethnic discrimination adds another problem to the environment that people deal with daily. People who reported discrimination have been shown to have a higher risk of high blood pressure and other stress-related physical effects. The many environmental, structural, and money-related stresses lead to more harm to mental and physical well-being. This causes poor health and disease.
People living in rural areas, especially poor rural areas, have access to fewer healthcare resources. Although 20% of the U.S. population lives in rural areas, only 9% of doctors practice there. People in rural areas usually have to travel longer distances for care. They also experience long waiting times at clinics. Or they might not be able to get the healthcare they need quickly. Rural areas with many Hispanic people have an average of 5.3 doctors per 10,000 residents. Non-rural areas have 8.7 doctors per 10,000 residents. Financial problems, like not having health insurance, are also common among the urban poor.
Differences in Access to Healthcare
There are many reasons for differences in getting healthcare. Some include:
- No regular doctor: Without a regular doctor, patients have more trouble getting care. They have fewer doctor visits and more trouble getting prescription drugs. Compared to white people, minority groups in the United States are less likely to have a doctor they see regularly. They are more likely to use emergency rooms and clinics as their main source of care. In the United Kingdom, this problem happens for a different reason. Since 2004, local doctors (GPs) are not responsible for care outside normal hours. This leads to many more visits to emergency departments.
- Lack of money: Not having enough money makes it hard for many Americans to get healthcare. But this problem seems to affect minority groups even more.
- Legal problems: Getting medical care for poor immigrant minorities can be stopped by legal rules about public insurance programs. For example, in the United States, federal law stops states from giving Medicaid coverage to immigrants who have been in the country for less than five years. Another example is when a person who doesn't speak English goes to a clinic where the receptionist doesn't speak their language. This is often seen in people who have limited English proficiency.
- System problems: These problems include poor transportation, not being able to schedule appointments quickly or at convenient times, and too much time spent waiting. All of these affect a person's ability and willingness to get needed care.
- Not enough doctors: In inner cities, rural areas, and communities with many minority people, getting medical care can be limited. This is because there are not enough primary care doctors, specialists, and testing facilities. This shortage can also include medical lab staff. Some areas have much less access to advanced tests and lab care. In the UK, Monitor (a public body) has a legal duty to make sure there are enough services in all parts of the country.
- How healthcare is paid for: The Institute of Medicine in the United States says that the way the U.S. healthcare system is broken up makes it hard to get care. Racial and ethnic minorities are more likely to have health insurance plans that limit what services are covered. They also offer a limited number of doctors.
- Language barriers: Language differences limit access to medical care for minorities in the United States who have limited English proficiency.
- Health knowledge: This is when patients have trouble getting, understanding, and using basic health information. For example, patients who don't understand good health might not know when to seek care for certain symptoms. While problems with health knowledge are not only in minority groups, the problem can be worse in these groups than in white people. This is due to money and education factors. A study in Mdantsane, South Africa, showed a link between a mother's education and her visits for pregnancy care. As patients have more education, they tend to use maternal healthcare services more.
- Lack of variety in healthcare workers: A main reason for differences in access to care is the cultural differences between mostly white healthcare providers and minority patients. Only 4% of doctors in the United States are African American, and only 5% are Hispanic. These percentages are much lower than their groups' share of the U.S. population.
- Age: Age can also be a factor in health differences. Many older Americans live on fixed incomes. This can make paying for healthcare hard. Also, they might face other problems like trouble moving around or no transportation. This makes getting healthcare physically challenging for them. Also, they might not be able to get health information online. Less than 15% of Americans over 65 have internet access. This could put older people at a disadvantage for getting important health information. On the other hand, older people in the U.S. (65 or older) get medical care through Medicare.
- Problems with traditional medicine and mental health treatments: Sometimes, traditional medicine and mental health treatments are not recognized or researched enough.
Health Insurance
A big part of the United States' healthcare system is health insurance. The main types of health insurance in the U.S. include government-funded health insurance and private health insurance. Government-funded insurance, paid for by taxes, includes Medicaid, Medicare, and CHIP. Private health insurance comes in many forms, like HMOs and Preferred Provider Organizations (PPOs). While health insurance makes healthcare more affordable in the U.S., problems with access and other issues create barriers to health equity.
Many problems with health insurance affect health equity:
- Understanding health insurance: Health insurance plans have common parts like premiums (yearly or monthly payments), deductibles (money you pay before insurance starts), co-payments, coinsurance, coverage limits, in-network versus out-of-network doctors, and prior approval. A survey found that only 9% of Americans understood these terms. To help people find insurance and understand policies, the Affordable Care Act (ACA) set up health insurance marketplaces. Here, people can compare different plans. Between 2014 and 2020, over 11.4 million people signed up for insurance through these marketplaces. However, most marketplaces focus on showing plans, not explaining the terms in detail.
- Lack of insurance: According to the Congressional Budget Office (CBO), 28.9 million people in the United States had no health insurance in 2018. That number was expected to rise to 35 million by 2029. Without health insurance, patients are more likely to delay medical care, go without needed care, go without prescription medicines, and be denied access to care. Minority groups in the United States have no insurance more often than white people. This problem does not exist in countries with fully funded public health systems, like the NHS in the UK.
- Not enough insurance: There are many reasons for not having enough insurance. A common reason is low premiums (the upfront yearly or monthly payment) and high deductibles (the money paid out of pocket before insurance pays). Under the ACA, people had to pay a fee if they didn't buy health insurance but could afford it. While this rule aimed to increase insurance rates, it also led many people to sign up for cheap plans that didn't provide enough coverage, just to avoid the fee. Like those with no insurance, these underinsured people also face problems from not getting enough care.
Dental Healthcare
In many countries, dental healthcare is harder to get than other kinds of healthcare. This leads to a higher risk for mouth and body diseases. In Western countries, there are dental care providers, and private or public healthcare systems usually help people get care. However, access is still limited for groups like homeless people, racial minorities, and those who are homebound or disabled. In Central and Eastern Europe, private dental care has led to a shortage of affordable options for lower-income people. In Eastern Europe, school children used to get care through school programs, but these have stopped. So, many children no longer have access to care.
Access to dental services and the range of services provided are much smaller in developing regions. Such services might only include emergency care and pain relief, ignoring preventative or restorative care. Regions like Africa, Asia, and Latin America don't have enough dental health professionals to meet people's needs. In Africa, for example, there is only one dentist for every 150,000 people. In developed countries, there's usually one dentist for every 2,000 people.
Differences in Healthcare Quality
Differences in the quality of healthcare exist. These are based on language, ethnicity, and race.
Problems with Talking to Doctors
Good communication is key for getting the right and effective treatment, no matter a patient's race. Bad communication can lead to wrong diagnoses, incorrect use of medicines, and not getting follow-up care. The relationship between a patient and doctor depends on both being able to talk well. Language and culture both play a big role in communication during a medical visit. Among patients, minorities have more trouble talking with their doctors. When surveyed, 19% of patients said they had problems talking with their doctors. This included understanding the doctor, feeling the doctor listened, and having questions but not asking them. In contrast, 33% of Hispanic people had problems talking with their doctor.
Communication is linked to health results. As communication gets better, patients are happier. This leads to them following advice more, and then to better health. The quality of care is affected if you can't talk with healthcare providers. Language is very important in communication. Efforts are needed to make sure patients and doctors talk well. For patients in the United States who don't speak English well, the language barrier is even bigger. Less than half of non-English speakers who say they need an interpreter during doctor visits report having one. Not having interpreters adds to the communication problem. Also, doctors not being able to talk with patients who don't speak English well leads to more tests, more serious procedures, and too many prescriptions. Language barriers have not only made it hard to schedule appointments, get prescriptions, and talk clearly, but have also been linked to worse health. This can be because people don't follow advice or delay seeking care, which can affect refugee health in the United States.
Many health places offer interpreter services for patients who don't speak English well. This helps when doctors don't speak the same language as the patient. However, there's growing evidence that patients need to talk with a doctor who speaks their language (not just an interpreter) to get the best medical care, feel connected to the doctor, and be happy with the care. Having patients and doctors who don't speak the same language might also lead to more medical spending and higher costs for the organization.
Other communication problems come from doctors not understanding different cultures. It's important for doctors to know about patients' health beliefs and practices without judging them. Understanding a patient's view of health and disease is important for diagnosis and treatment. So, doctors need to check patients' health beliefs and practices to improve care quality. Patients' health decisions can be affected by religious beliefs, not trusting Western medicine, and family roles. A white doctor might not know about these things.
Doctor Discrimination
Doctor discrimination happens when healthcare providers, either without knowing it or on purpose, treat certain racial and ethnic patients differently from others. This might be because of stereotypes doctors have about ethnic or racial groups. A 2000 study suggested that doctors might be more likely to link negative racial stereotypes to their minority patients. This can happen no matter their education, income, or personality. Two types of stereotypes might be involved: automatic stereotypes or goal-modified stereotypes. Automatic stereotyping is when stereotypes are used without thinking and affect decisions. Goal-modified stereotyping is more conscious. It happens when doctors need to fill in information quickly to make decisions. Doctors might not even know they have these hidden biases.
Some research suggests that ethnic minorities are less likely than white people to get a kidney transplant once on dialysis. They are also less likely to get pain medicine for broken bones. Critics question this research and say more studies are needed to see how doctors and patients make treatment decisions. Others argue that certain diseases happen more often in certain ethnic groups, and that medical decisions don't always show these differences.
Lack of Preventative Care
According to a 2009 report, Americans without health insurance are less likely to get preventative health services. For example, minorities are not regularly checked for colon cancer. The death rate for colon cancer has gone up among African American and Hispanic people. Also, patients who don't speak English well are less likely to get preventative health services like mammograms. Studies have shown that using professional interpreters has greatly reduced differences in rates of stool tests, flu shots, and Pap smears. In the UK, Public Health England, a free service that is part of the NHS, offers regular checks to anyone in a high-risk group (like people over 45) for major diseases (like colon cancer or diabetic eye problems).
How to Achieve Health Equity
Many ways exist to achieve health equity and reduce differences. Some examples include:
- Speaking up: Speaking up for health equity is a key way to push for good policy changes. A study found that certain types of information are more convincing. Also, sharing knowledge can increase how much it's used. There are many different people who can speak up and many different targets for their efforts. Speaking up needs to be planned for each situation.
- Rewards for doctors: One reason for health unfairness is that non-white patients are treated differently than white patients. Giving doctors rewards to create more equal treatment is one idea to remove doctor bias. These rewards are usually money because it works well to influence how doctors act.
- Using Evidence Based Medicine (EBM): EBM shows promise in reducing doctor bias, which helps health equity. In theory, EBM can reduce differences. However, other research suggests it might make them worse. Some problems mentioned include EBM making decisions too strict and its origins as a purely cost-driven measure.
- Increasing awareness: The most common way to improve health equity is to increase public awareness. Not enough public awareness is a main reason why there haven't been big improvements in reducing health differences in ethnic and minority groups. More public awareness would lead to more awareness in government, more data on differences, and more research into the problem.
- Evaluating policies: It's very hard to know which policies and actions are best at reducing health inequalities. So, it's important that policies and actions meant to affect health fairness are better evaluated. The Gradient Evaluation Framework (GEF) is a tool that can be used to see if policies will lead to more health equity among children and their families.
- The AIM framework: In a small study, researchers looked at how AIM (ability, incentives, and management feedback) helped reduce differences in finding pressure ulcers between African American and Caucasian residents. The results showed that providing training, money rewards, and feedback helped successfully reduce pressure ulcers. Specifically, the gap in finding them between the two groups got smaller. Researchers suggested more studies over longer times to check how well the AIM framework works.
- Watching social factors: In 2017, the World Health Organization and UNICEF called for tracking actions on the social factors that affect health. This was to ensure countries kept their promises from a declaration on social factors of health. This tracking helps improve health equity.
- Changing how health services are given: Health services play a big role in health equity. Health unfairness comes from not being able to get care due to poor money status and other social determinants of health. Most high-quality health services go to wealthy people, leaving poor people with limited choices. To change this and move towards health equity, healthcare needs to increase in areas or neighborhoods with low-income families and individuals.
- Making treatment for the poor a priority: Because of the challenges of getting healthcare with low income, many illnesses and injuries go untreated or don't get enough treatment. Making treatment a priority for the poor will give them the resources they need to be healthy, because health is a basic human right.
- Using different types of medicine: The big differences between city medicine and alternative medicine show the need for a system that serves both types of people. City medicine generally believes that technology is the best way to treat illness. Alternative medicine relies more on natural remedies. It believes that city hospitals are not best for individual needs. So, using different types of medicine is a good plan for communities with Indigenous people and mixed rural-urban populations. This approach understands the needs of different people and is a step closer to health equity. It avoids the extremes of most current healthcare methods. It provides a middle ground for health problems not solved by one type of health care alone. By using integrative medicine, long-term and unsolved health issues are better treated. This borrows from both technological and philosophical approaches. This idea is being considered in countries with diverse communities, like many Latin American countries with large indigenous populations.
- Artificial Intelligence (AI): AI can help find and improve health differences. A recent review found that it's important to work with different communities when developing AI health apps. These apps should also be checked for biases that are found later.
- Pandemic Treaty: In 2023, the WHO's member states made health equity the main goal of a new international agreement being discussed.
G20's Healthcare Plan
In 2023, the G20, with the Government of Andhra Pradesh, India, opened a 100-bed hospital in Srikakulam. This was part of its Affordable Healthcare Model Hospital plan. It received support from the Aarogyasri scheme.
Health Inequalities
Health inequality is a term used in some countries. It refers to cases where the health of two groups (not always ethnic or racial) is different, even if they have similar access to healthcare. Examples include higher rates of sickness and death for people in lower-status jobs than those in higher-status jobs. Also, people from ethnic minorities are more likely to be diagnosed with a mental health disorder. In Canada, this issue was brought to public attention by the LaLonde report.
In the UK, the Black Report was created in 1980 to highlight inequalities. On February 11, 2010, Sir Michael Marmot, a health expert, published the Fair Society, Healthy Lives report. It was about the link between health and poverty. Marmot said his findings showed a "social gradient in health." This means the poorest people live seven years shorter lives than the wealthiest. The poor are also more likely to have a disability. In its report on this study, The Economist said that the reasons for this health inequality include unhealthy lifestyles. Smoking is still more common, and obesity is growing fastest, among the poor in Britain.
In June 2018, the European Commission launched the Joint Action Health Equity in Europe. Forty-nine groups from 25 European Union countries will work together. Their goal is to address health inequalities and the underlying social determinants of health across Europe. This project aims to achieve greater fairness in health in Europe for all social groups. It also seeks to reduce differences between countries in how they tackle health inequalities.
See also
- Biological inequity
- Center for Minority Health
- Drift hypothesis
- EuroHealthNet
- Environmental justice
- Food Justice Movement
- Global health
- Global Task Force on Expanded Access to Cancer Care and Control in Developing Countries
- Health care
- Health-related embarrassment
- Health Disparities Center
- Health inequality in the United Kingdom
- Healthcare and the LGBT community
- Hopkins Center for Health Disparities Solutions
- Immigrant paradox
- Inequality in disease
- Inverse care law
- Mental health inequality
- Population health
- Public health
- Publicly funded health care
- Single-payer healthcare
- Social determinants of health
- Social determinants of health in poverty
- Unnatural Causes: Is Inequality Making Us Sick?
- Weathering hypothesis
 | John T. Biggers |
 | Thomas Blackshear |
 | Mark Bradford |
 | Beverly Buchanan |